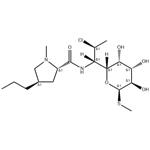
Clindamycin
- Product NameClindamycin
- CAS18323-44-9
- CBNumberCB4399999
- MFC18H33ClN2O5S
- MW424.98
- EINECS242-209-1
- MDL NumberMFCD00072005
- MOL File18323-44-9.mol
- MSDS FileSDS
Chemical Properties
| alpha | D +214° (chloroform) |
| Boiling point | 134°C (rough estimate) |
| Density | 1.1184 (rough estimate) |
| refractive index | 1.6100 (estimate) |
| storage temp. | Store at -20°C |
| solubility | DMSO:52.5(Max Conc. mg/mL);123.54(Max Conc. mM) DMF:30.0(Max Conc. mg/mL);70.59(Max Conc. mM) Ethanol:52.5(Max Conc. mg/mL);123.54(Max Conc. mM) PBS (pH 7.2):0.2(Max Conc. mg/mL);0.47(Max Conc. mM) |
| form | A crystalline solid |
| pka | 7.6(at 25℃) |
| color | White to light yellow |
| BCS Class | 1 |
| Stability | Hygroscopic |
| InChIKey | KDLRVYVGXIQJDK-GWOVNWBCNA-N |
| SMILES | [C@]([H])([C@]1([H])[C@@H]([C@H](O)[C@@H](O)[C@@H](SC)O1)O)([C@@H](Cl)C)NC([C@H]1N(C[C@H](CCC)C1)C)=O |&1:0,2,4,5,7,9,14,19,22,r| |
| CAS DataBase Reference | 18323-44-9(CAS DataBase Reference) |
| FDA UNII | 3U02EL437C |
| ATC code | D10AF01,D10AF51,G01AA10,J01FF01 |
| EPA Substance Registry System | L-threo-?-D-galacto-Octopyranoside, methyl 7-chloro-6,7,8-trideoxy-6-[[[(2S,4R)-1-methyl-4-propyl-2-pyrrolidinyl]carbonyl]amino]-1-thio- (18323-44-9) |
Safety
| Symbol(GHS) |
 
|
|||||||||
| Signal word | Warning | |||||||||
| Hazard statements | H362-H319 | |||||||||
| Precautionary statements | P201-P260-P263-P264-P270-P308+P313-P264-P280-P305+P351+P338-P337+P313P | |||||||||
| Hazardous Substances Data | 18323-44-9(Hazardous Substances Data) | |||||||||
| Toxicity | LD50 subcutaneous in rat: 2618mg/kg | |||||||||
| NFPA 704: |
|