Various applications and degradation properties of polyvinyl alcohol
General description
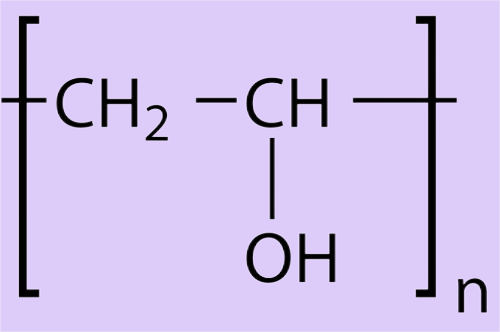
Polyvinyl alcohol (PVA) is a linear synthetic polymer produced via partial or full hydrolysis of polyvinyl acetate to remove the acetate groups. The amount of hydroxylation determines the physical characteristics, chemical properties, and mechanical properties of the PVA[1]. The resulting PVA polymer is highly soluble in water but resistant to most organic solvents. The higher the degree of hydroxylation and polymerization of the PVA, the lower the solubility in water and the more difficult it is to crystallize[2]. Due to its water solubility, PVA needs to be crosslinked to form hydrogels for use in several applications. The crosslinks, either physical or chemical, provide the structural stability the hydrogel needs after it swells in the presence of water or biological fluids.3 The degree of crosslinking dictates the amount of fluid uptake, and thus the physical, chemical, and diffusional properties of the polymer, and ultimately its biological properties[3].

Polyvinyl alcohol (PVA) is a synthetic polymer derived from polyvinyl acetate through partial or full hydroxylation. PVA is commonly used in medical devices due to its low protein adsorption characteristics, biocompatibility, high water solubility, and chemical resistance[4-5]. Some of the most common medical uses of PVA are in soft contact lenses, eye drops, embolization particles, tissue adhesion barriers, and as artificial cartilage and meniscus. The purpose of this review is to evaluate the available published information on PVA with respect to its safety as a medical device implant material for cartilage replacement[6].
Historical use of pva for medical devices
PVA's resistance against organic solvents and aqueous solubility makes it adaptable for many applications. PVA is commonly used in the textile industries, for paper products manufacturing, in the food packaging industry, and as medical devices. PVA is used as an industrial and commercial product due to its low environmental impact, which includes its high chemical resistance, aqueous solubility, and biodegradability[7-8]. FDA has approved PVA to be in close contact with food products; in fact, PVA films exhibit excellent barrier properties for food packaging systems. In medical devices, PVA is used as a biomaterial due to its biocompatible, nontoxic, noncarcinogenic, swelling properties, and bioadhesive characteristics. Table I identifies some implant and nonimplant devices currently made of different forms of PVA.
PVA hydrogels and membranes have been developed for biomedical applications such as contact lenses, artificial pancreases, hemodialysis, and synthetic vitreous humor, as well as for implantable medical materials to replace cartilage and meniscus tissues[9]. It is an attractive material for these applications because of its biocompatibility and low protein adsorption properties resulting in low cell adhesion compared with other hydrogels. PVA shows higher tensile strength and elongation before breaking than hydrogels such as polyhydroxyethyl methacrylate, making PVA a suitable hydrogel for soft contact lenses, extending wearing time without inducing hypoxia to the cornea[10].
Low-temperature crystallization of PVA with a water miscible organic solvent has been used to produce a hydrogel with high tensile strength, high water content, and low protein adsorption, further improving its use as a lens material. PVA has also been used in combination with polyethylene glycol and hydroxypropyl methylcellulose, increasing content for medical applications such as artificial tears[11].
In addition to its use in nonimplanted medical applications, PVA is used in several medical devices that are implanted in the body. Particulate PVA has been used to treat vascular embolisms, hydrophilic coatings to improve neurologic regeneration, and as tissue adhesion barriers. These diverse uses of PVA in medical devices indicate that it is safe for human use in applications where adsorption of host protein is undesired and the device experiences tensile stress during use[12]. PVA's properties also make it a good biomaterial candidate for simulating natural tissues inside the body, such as cartilage and meniscus. The following sections will review PVA implants for cartilage replacement applications.
Pva for cartilage replacement in articular and meniscal applications
Cartilage lacks vascularity, and its cellular components, chondrocytes, have low mitotic ability, making it a particularly difficult tissue to repair or regenerate[13]. Cartilage is the prototypical, biologic hydrogel composed of ∼60%–80% water with its mass balance being mostly collagen and glycosaminoglycans. PVA hydrogels have been investigated for replacement of damaged cartilage due to their high water content, as well as their elastic and compressive mechanical properties. PVA cryogels used in cartilage resurfacing are prepared from high concentrations of high-molecular weight polymers (generally 30% PVA or higher). These PVA cryogels have water contents similar to the surrounding healthy cartilage and when prepared from saline are osmotically balanced with the fluids and tissues within the joint space[14]. Bray and Merrill were one of the first groups to report the use of PVA for articular cartilage repair in the early 1970s. There are many other researchers who followed and studied PVA as an artificial cartilage repair; we will address some of them below[15].
Articular cartilage consists of a lubricated, avascular tissue with high water content and mechanical tensile strength of 17 MPa and compressive modulus varying between 0.53 and 1.82 MPa. An ideal implant replacement for cartilage would mimic this structure, mechanical properties, and composition[16]. Total joint replacement and total shoulder arthroplasty are commonly performed using polyethylene and/or metallic materials (titanium, chromium, etc.), which are both stiffer than cartilage and do not have lubrication, shock absorption, and deformation properties of native cartilage[17]. Although they are suitable as joint replacement devices, not all cartilage defects require radical tissue removal to achieve restoration of function. PVA hydrogels have been investigated as artificial cartilage replacements due to their rubber elastic physical properties, and because the hydrogels can be manufactured to have tensile strength in the cartilage range of 1–17 MPa and compressive modulus varying from 0.0012 and 0.85 MPa depending on the polymer concentration and number of cycles tested[18].
Preclinical and clinical studies using PVA hydrogels
The biocompatibility of PVA implants was demonstrated by Tadavarthy et al. in 1975 with the development of the Ivalon embolic material. PVA gels with 80%–90% water content by weight were implanted subcutaneously or intramuscularly into rabbits, and no adverse effects were noticed in the surrounding tissue leading to a confirmation of the biocompatibility of the material[19]. PVA hydrogel crosslinked by gamma irradiation has also been shown to function as a vitreous substitute. In these studies, PVA hydrogels were injected into the eyes of crab-eating macaques; after 3 months, there was no evidence of tissue loss, changes in opthalmoscopic findings, or increases in intraocular pressure[20].
Biocompatibility of PVA particles used for vein embolization was studied by Covey et al. in 58 patients, determining that the particles were safe and effective in achieving left hemi-liver hypertrophy. Nakamura et al. studied PVA-H in rats and reported the formation of a malignant tumor; this is one of the only reports with carcinogenesis results[21-22]. It was noted by Nakamura that this carcinogenesis formation might be due to the high water content in PVA-H. In the food industry, PVA's oral toxicity was reviewed by DeMerlis and Schoneker concluding that PVA is an orally safe product to use. The LD50 reported was between 15 and 20 g/kg, indicating a low acute oral toxicity[23].
Preclinical and clinical studies using PVA hydrogels for orthopedic applications
In orthopedics, PVA implants have been used in meniscus and cartilage replacements. Kobayashi et al. studied PVA hydrogel for the replacement of meniscus using a rabbit model. The PVA hydrogel implants were placed in the lateral compartment of one knee of female rabbits[24]. A meniscectomy on the bilateral knee of the same rabbit was done as a control. Five rabbits were examined after 2 years, while the rest were examined at earlier time points. Results of the 2-years postoperative follow-up showed that the PVA hydrogel implants were intact, with no wear or dislocation seen. The PVA hydrogel implants were shown to be stable inside the body and prevented osteoarthritic change in the surrounding articular cartilage. PVA hydrogel was also implanted in white rabbits for up to 52 weeks as an artificial articular cartilage replacement resulting in low inflammatory responses and high in vivo biocompatibility[25-26].
References
[1] A.A. Alfi, S.D. Al-Qahtani, N.M. Alatawi, R.M.S. Attar, K. Abu Al-Ola, T.M. Habeebullah, N.M. El-Metwaly, Simple preparation of novel photochromic polyvinyl alcohol/carboxymethyl cellulose security barcode incorporated with lanthanide-doped aluminate for anticounterfeiting applications, Luminescence 37(7) (2022) 1152-1161.
[2] A. Bouzidi, W. Jilani, T.H. AlAbdulaal, M. Jalalah, F.A. Harraz, I.S. Yahia, M.A. Ibrahim, H.Y. Zahran, Simple synthesis and characterization of novel polyvinyl alcohol capped sodium selenite solid composite film (PVA: NaSe SCF) samples, J. Sci.: Adv. Mater. Devices 7(3) (2022) 100458.
[3] Charlena, T. Kemala, Ravena, Coating of nanotube Ti6Al4V alloy with hydroxyapatite-chitosan-polyvinyl alcohol composite, Indones. J. Fundam. Appl. Chem. 7(2) (2022) 58-67.
[4] H.Y. Chi, N.Y. Chang, C. Li, V. Chan, J.H. Hsieh, Y.-H. Tsai, T. Lin, Fabrication of Gelatin Nanofibers by Electrospinning-Mixture of Gelatin and Polyvinyl Alcohol, Polymers (Basel, Switz.) 14(13) (2022) 2610.
[5] T. Engstrand, B.T. Melander, Pharmaceutical compositions and medical treatments for blocking or inhibiting semicarbazide sensitive amine oxidase (SSAO) or SSAO derived substances, PVAC Medical Technologies Ltd., Cyprus . 2021, p. 28pp.
[6] F. Gharbi, K. Benthami, T.H. Alsheddi, M.M.E. Barakat, N. Alnaim, A. Alshoaibi, S.A. Nouh, Structural, Thermal, and Optical Studies of Gamma Irradiated Polyvinyl Alcohol-, Lignosulfonate-, and Palladium Nanocomposite Film, Polymers (Basel, Switz.) 14(13) (2022) 2613.
[7] G. Goksen, M.J. Fabra, A. Perez-Cataluna, H.I. Ekiz, G. Sanchez, A. Lopez-Rubio, Biodegradable active food packaging structures based on hybrid cross-linked electrospun polyvinyl alcohol fibers containing essential oils and their application in the preservation of chicken breast fillets, Food Packag. Shelf Life 27 (2021) 100613.
[8] J. Guo, L. Yang, L. Zhang, C. Li, Simultaneous exfoliation and functionalization of black phosphorus by sucrose-assisted ball milling with NMP intercalating and preparation of flame retardant polyvinyl alcohol film, Polymer 255 (2022) 125036.
[9] F. Hu, H. Lu, G. Xu, L. Lv, L. Chen, Z. Shao, Carbon quantum dots improve the mechanical behavior of polyvinyl alcohol/polyethylene glycol hydrogel, J. Appl. Polym. Sci. (2022) Ahead of Print.
[10] J. Huang, G. Yadav, D.E. Turney, J. Cho, M. Nyce, B.R. Wygant, T.N. Lambert, S. Banerjee, Ion-Selective Graphene Oxide/Polyvinyl Alcohol Composite Membranes for Rechargeable Alkaline Zinc Manganese Dioxide Batteries, ACS Appl. Energy Mater. (2022) Ahead of Print.
[11] C. Jiang, A kind of fully degradable flame for high-toughness polyvinyl alcohol composite material and preparation method thereof [Machine Translation], Wurui New Material Technology Jiangsu Co., Ltd., Peop. Rep. China . 2022, p. 12pp.
[12] H. Kamata, Y. Nishiumi, H. Kabayama, Metal adsorption fiber and manufacturing method of metal adsorption fiber [Machine Translation], Kuraray Co., Ltd., Japan . 2022.
[13] P.S. Kanavi, S. Meti, R.H. Fattepur, V.B. Patil, Influence of Copper Oxide Nanoparticles on AC Conductivity of Polyvinyl Alcohol-Polyaniline Polymer Blends, J. Electron. Mater. (2022) Ahead of Print.
[14] D. Kong, Z.M. El-Bahy, H. Algadi, T. Li, S.M. El-Bahy, M.A. Nassan, J. Li, A.A. Faheim, A. Li, C. Xu, M. Huang, D. Cui, H. Wei, Highly sensitive strain sensors with wide operation range from strong MXene-composited polyvinyl alcohol/sodium carboxymethylcellulose double network hydrogel, Adv. Compos. Hybrid Mater. (2022) Ahead of Print.
[15] C. Kouderis, S. Tsigoias, P. Siafarika, A.G. Kalampounias, Acoustically induced birefringence in polymer aqueous solutions: The case of polyvinyl alcohol, Phys. B (Amsterdam, Neth.) 643 (2022) 414189.
[16] G. Li, J. Zhao, Z. Wang, X. Yu, T. Zhao, X. Liang, R. Sun, L. Cao, P. Zhu, Ultrathin, flexible, conductive silver nanowires@polyvinyl alcohol composite film fabricated via the combination of air plasma treatment and thermal sintering for electromagnetic interference shielding, Mater. Lett. 325 (2022) 132814.
[17] Y. Li, H. Cao, W. Liu, P. Liu, Effective degradation of tetracycline via recyclable cellulose nanofibrils/polyvinyl alcohol/Fe3O4 hybrid hydrogel as a photo-Fenton catalyst, Chemosphere 307(Part_1) (2022) 135665.
[18] S. Lu, B. Ouyang, S. Han, F. Qiao, K. Chen, F. Wu, A. Xie, E. Kan, H. Zeng, Flexible Polypyrrole Nanotube-Polyethylene Glycol-Polyvinyl Alcohol Hydrogels for Enhanced Electromagnetic Shielding, ACS Appl. Nano Mater. (2022) Ahead of Print.
[19] J. Morand, S. Mollov, An integrated cooling liquid cavity in a printed circuit board and a method to make the same, Mitsubishi Electric R & D Centre Europe B.V., Neth.; Mitsubishi Electric Corporation . 2022, p. 15pp.
[20] Y. Okano, Binder for building materials [Machine Translation], Wetlab Holding K. K., Japan . 2022.
[21] M.-B. Roman, F. Oancea, D. Constantinescu-Aruxandei, Controlled-release fertilizer composition and process for preparing the same, FIA-Crop Control S.r.l., Rom. . 2022.
[22] H. Sun, W. Zhao, Z. Chen, B. Tian, H. Li, Q. Li, Curative effect of modified injection of polyvinyl alcohol foam hardening agent on varicose great saphenous vein, Xibei Guofang Yixue Zazhi 41(11) (2020) 23-27.
[23] S. Wang, H. Liu, L. Xie, Y. Li, A kind of polyvinyl alcohol-fluorene based nano sheet composite film and preparation method thereof [Machine Translation], Nanjing University of Posts and Telecommunications, Peop. Rep. China . 2022, p. 13pp.
[24] H. Xia, Y. Zhang, H. Xin, D. Yan, G. Li, R. Chen, Metal-phenolic network-based polydopamine@Cu within a polyvinyl alcohol hydrogel film for improved infected wound healing through antibacterial and pro-angiogenesis activity, Mater. Des. 221 (2022) 110904.
[25] S.J. Yeo, S. Chaudhari, U. Kim, H. Shin, K.Y. Cho, H.T. Kwon, M. Shon, S. Nam, Y. Park, Robust and water-selective natural-cellulose-nanofiber-reinforced polyvinyl alcohol composite membranes for pervaporation of isopropanol/water mixtures, Chem. Eng. Process. 179 (2022) 109046.
[26] Y. Zhang, Experimental study on compression performance of polyvinyl alcohol fiber recycled aggregate concrete, Zhongyuan Gongxueyuan Xuebao 32(1) (2021) 63-68.
Related articles And Qustion
See also
Lastest Price from Poly(vinyl alcohol) manufacturers

US $0.00/kg2025-09-19
- CAS:
- 9002-89-5
- Min. Order:
- 25kg
- Purity:
- 99%
- Supply Ability:
- 20MT

US $0.00-0.00/KG2025-07-16
- CAS:
- 9002-89-5
- Min. Order:
- 1KG
- Purity:
- 98%min
- Supply Ability:
- 30tons/month