Unveiling Lambrolizumab: A Comprehensive Insight into Its Production, Mechanism, and Clinical Implications
Introduction
Lambrolizumab, prominently recognized as Pembrolizumab in the medical community, marks a transformative stride in the field of immunotherapy, establishing a new frontier in cancer treatment. This innovative therapeutic agent is primarily utilized to counter a spectrum of cancers, showcasing its versatility and potency in the oncological landscape.
As a monoclonal antibody, Lambrolizumab operates by fine-tuning the human immune system, a sophisticated biological defense mechanism evolved to protect the body from various threats, including malignancies. By specifically targeting and inhibiting the programmed cell death protein 1 (PD-1) pathway, Lambrolizumab dismantles the cancer cell's ability to evade immune detection, effectively 'unmasking' them to the vigilant eyes of the immune system.
This mechanism not only amplifies the immune system's capacity to identify and assault cancer cells but also signifies a paradigm shift in cancer treatment. Traditional therapies often adopt a brute-force approach, targeting rapidly dividing cells indiscriminately and culminating in a plethora of side effects. In contrast, Lambrolizumab's precision-guided modality offers a more targeted, and consequently, a more patient-friendly approach to cancer therapy[1].
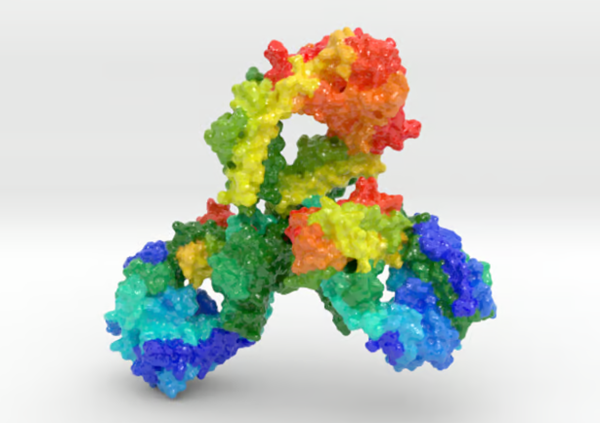
Fig. 1 Characteristics of Lambrolizumab
Production Method
The production of Lambrolizumab, a biopharmaceutical marvel, involves complex biotechnological processes, harnessing recombinant DNA technology to produce monoclonal antibodies. This process begins with the genetic engineering of mammalian cells, typically Chinese hamster ovary (CHO) cells, which are widely used due to their robust growth and protein production capabilities.
Cell Line Development
The initial step involves introducing the gene encoding the Lambrolizumab antibody into CHO cells. This is achieved through transfection, whereby a vector carrying the gene is inserted into the cell nucleus, enabling the cells to produce the antibody.
Cultivation
Post-transfection, the engineered CHO cells are cultivated in bioreactors, controlled environments where conditions such as temperature, pH, and nutrient supply are meticulously regulated to optimize cell growth and antibody production.
Harvesting and Purification
Once the cells produce a sufficient quantity of antibodies, the bioreactor's contents are harvested. The mixture then undergoes a series of purification steps, including chromatography and filtration, to isolate the Lambrolizumab antibodies from other cellular components.
Quality Control
Ensuring the purity and functionality of Lambrolizumab is paramount. Rigorous quality control tests are conducted to verify the absence of contaminants and to confirm that the antibodies meet predefined efficacy and safety standards[2].
Scaling Up
The production process is scalable, allowing for the transition from small-scale laboratory production to large-scale commercial manufacturing, which is essential for meeting the global demand for this therapeutic agent.
Mechanism of Action
Cancer evolves to exploit multiple mechanisms in order to avoid immune-cell recognition and antitumor effector functions, thereby limiting the clinical benefits of immunotherapy strategies. Antibodies that block the inhibitory receptor cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4), such as ipilimumab, have been shown to release one of these negative immune regulatory pathways, leading to durable responses in a subgroup of patients with metastatic melanoma and an overall survival benefit in patients with metastatic melanoma. The programmed cell death 1 (PD-1) receptor is another inhibitory receptor expressed by T cells preferentially with long-term exposure to antigens. Its primary ligand, PD-L1 (also known as B7-H1 or CD274), is frequently expressed within the tumor microenvironment, including cancer cells and tumor-infiltrating macrophages. The PD-1 receptor has a second ligand, PD-L2 (also known as B7-DC or CD273), that is preferentially expressed by antigen-presenting cells. In tumor models, PD-1 negatively regulates the effector phase of T-cell responses after ligation of PD-L1 expressed within the tumor. It has been postulated that antibodies that block the interaction between PD-1 and PD-L1 in tumors may preferentially release the cytotoxic function of tumor-specific T cells with fewer systemic toxic effects than those that are seen with other immune checkpoint inhibitors.
Two large, dose-escalation, phase 1 clinical trials evaluating the safety of the anti–PD-1 antibody nivolumab (formerly known as BMS936558) and the anti–PD-L1 antibody BMS936559 showed significant antitumor activity in patients with advanced melanoma, lung carcinoma, and renal-cell carcinoma, among other cancers, thus validating the PD-1–PD-L1 axis as a therapeutic target. Most tumor responses were durable beyond 1 year. Toxic effects were generally of low grade.
Lambrolizumab (previously known as MK-3475) is a highly selective, humanized monoclonal IgG4–kappa isotype antibody against PD-1 that is designed to block the negative immune regulatory signaling of the PD-1 receptor expressed by T cells. The variable region sequences of a very-high-affinity mouse antihuman PD-1 antibody (dissociation constant, 28 pM) were grafted into a human IgG4 immunoglobulin with a stabilizing S228P Fc alteration. The IgG4 immunoglobulin subtype does not engage Fc receptors or activate complement, thus avoiding cytotoxic effects of the antibody when it binds to the T cells that it is intended to activate. In T-cell activation assays that used human donor blood cells, the 50% effective concentration was in the range of 0.1 to 0.3 nM (unpublished data). The first dose-escalation phase 1 study involving patients with solid tumors showed that lambrolizumab was safe at the dose levels tested (1 mg per kilogram of body weight, 3 mg per kilogram, and 10 mg per kilogram, administered every 2 weeks) without reaching a maximum tolerated dose. In addition, clinical responses were observed at all the dose levels.
Side Effects
Among 133 pts who were dosed with lambrolizumab before July 31, 2012, and evaluable for adverse events (AEs) as of September 28, 2012, fatigue (22%), rash (18%), and pruritus (14%) were the most common drug-related AEs (mostly grade 1/2). The incidence of drug-related grade 3/4 AEs was 10% (24% regardless of attribution). Four drug-related cases of pneumonitis were reported, all of grade 1/2. Grade 3/4 drug-related hypothyroidism (n = 1) and hyperthyroidism (n = 1) were noted.
Preliminary data suggest that lambrolizumab has significant antitumor activity and is well tolerated with manageable side effects in both IPI-naive and IPI-pretreated MEL pts. These data have led to an ongoing, international, randomized study of lambrolizumab versus chemotherapy in IPI-pretreated MEL[3].
References
[1]Hamid O, Robert C, Daud A, et al. Safety and tumor responses with lambrolizumab (anti–PD-1) in melanoma[J]. New England Journal of Medicine, 2013, 369(2): 134-144.
[2]Mandel J J, Olar A, Aldape K D, et al. Lambrolizumab induced central nervous system (CNS) toxicity[J]. Journal of the neurological sciences, 2014, 344(1): 229-231.
[3]Ribas A, Robert C, Daud A, et al. Clinical efficacy and safety of lambrolizumab (MK-3475, Anti-PD-1 monoclonal antibody) in patients with advanced melanoma[J]. 2013.
Related articles And Qustion
See also

US $0.00/MG2025-04-21
- CAS:
- 1374853-91-4
- Min. Order:
- 500MG
- Purity:
- 98%min
- Supply Ability:
- 30KG/month

US $0.00/g2024-09-25
- CAS:
- 1374853-91-4
- Min. Order:
- 10g
- Purity:
- 99%
- Supply Ability:
- 50kg