The Comprehensive Guide to Rituximab: Mechanisms, Applications, and Care
Introduction
Rituximab, a pioneering chimeric monoclonal antibody, has been a beacon of hope in the realms of oncology and immunology. Designed to target CD20-positive B cells, it offers a novel approach to treating various conditions that were previously challenging to manage. Its introduction into the medical field has not only provided patients with new hope but has also spurred a wave of innovation in therapeutic strategies. This article aims to dissect the multifaceted aspects of Rituximab, exploring its mechanism of action, its diverse applications, the spectrum of side effects, and its storage protocols, all through the lens of a chemical professional[1].

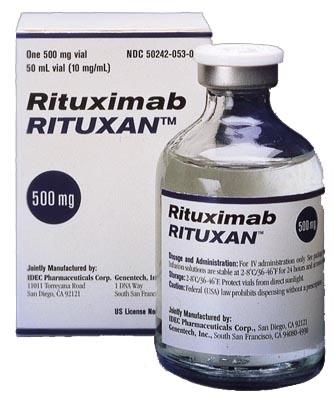
Fig. 1 Characteristics of Rituximab
Mechanism of Action
Rituximab has become a mainstay in the therapy of a broad variety of B-cell malignancies. In some B-cell malignancies, rituximab alone can induce high response rates and long-term remissions, while in others, adding rituximab to chemotherapy enhances the rates of complete response, long-term remission, and cure. Despite its undeniable value as a component of therapy for B-cell malignancies, rituximab is not effective for all patients, and development of resistance to therapy is common. Understanding the mechanisms by which rituximab induces anti-tumor responses is central to our ability to improve on what is already a highly effective therapy.
We know that anti-cancer monoclonal antibodies (mAbs) can mediate anti-tumor effects by a variety of mechanisms, including signaling resulting in cell cycle arrest, direct induction of apoptosis, and sensitization to cytotoxic drugs, complement-mediated cytotoxicity (CMC) and antibody-dependent cellular cytotoxicity (ADCC). Ideally, we would study these, and any other, mechanisms of action of rituximab using experimental conditions that reflect clinical therapy. In reality this is more easily said than done. As a single agent, rituximab is usually administered weekly for 4 weeks. When used in combination with chemotherapy, it is often administered every 3 to 4 weeks. The pharmacokinetics of rituximab is similar to that seen with human IgG. Thus, whether given weekly or monthly, rituximab is present at therapeutic levels in the circulation of patients for months at a time. As an IgG, rituximab distributes in both the intravascular and extravascular compartments, and so should be present within involved lymph nodes with their complex architecture in an environment that includes not only malignant B cells but also stromal cells, benign lymphocytes, extracellular matrix, vasculature, proteins in the extravascular fluid, and a complex mixture of cytokines and chemokines.
The mechanism of action of Rituximab is a testament to the elegance of targeted therapy in modern medicine. By zeroing in on the CD20 antigen on B cells, Rituximab initiates a cascade of immunological events leading to the selective depletion of these cells. This process is crucial in diseases where B cells play a pivotal role, whether they are malignantly transformed or pathologically active in autoimmune disorders. The antibody-dependent cellular cytotoxicity (ADCC) mechanism is particularly notable, where Rituximab binds to CD20 and recruits immune effector cells to induce the lysis of the target cell. Additionally, complement-dependent cytotoxicity (CDC) plays a role, where Rituximab activation leads to the complement cascade, culminating in cell destruction. These mechanisms highlight the sophisticated interplay between the therapeutic agent and the immune system, offering a targeted approach to treatment that spares non-target cells, thus reducing collateral damage[2].
Applications
The therapeutic applications of Rituximab are extensive and varied. In oncology, its efficacy in treating B-cell malignancies, such as Non-Hodgkin's Lymphoma (NHL) and Chronic Lymphocytic Leukemia (CLL), has been well-documented. These malignancies, which were once daunting challenges, are now met with a targeted approach that offers improved outcomes and new hope for patients. Beyond oncology, Rituximab has made significant strides in the treatment of autoimmune diseases. In conditions like Rheumatoid Arthritis (RA) and Systemic Lupus Erythematosus (SLE), Rituximab has provided a therapeutic option when traditional treatments have failed, demonstrating its versatility and effectiveness. The expanding applications of Rituximab in medicine are a testament to the ongoing research and clinical trials that continue to uncover its potential in treating a broader spectrum of diseases[3].
Side Effects
The early studies confirmed the tolerable side-effect profile of rituximab, with the only common serious events being infusion-related hypotension, fever and rigors, seen almost entirely with the first infusion and not recurring on continued treatment. Patients with large numbers of circulating lymphoma cells are more likely to suffer adverse effects, probably mediated by complement activation. The antibody has a substantial effect upon the numbers of circulating normal B-cells, but these recover after an interval of 3 – 6 months and there is consequently little impact upon immunoglobulin levels. The incidence of opportunistic infection is low[3].
References
[1]Onrust S V, Lamb H M, Barman Balfour J A. Rituximab[J]. Drugs, 1999, 58: 79-88.
[2]Weiner G J. Rituximab: mechanism of action[C]//Seminars in hematology. WB Saunders, 2010, 47(2): 115-123.
[3]Johnson P W M, Glennie M J. Rituximab: mechanisms and applications[J]. British journal of cancer, 2001, 85(11): 1619-1623.
Related articles And Qustion
Lastest Price from Rituximab manufacturers
US $0.00/G2025-04-21
- CAS:
- 174722-31-7
- Min. Order:
- 1G
- Purity:
- 98%min
- Supply Ability:
- 30kg/month

US $1.10/g2021-07-02
- CAS:
- 174722-31-7
- Min. Order:
- 1g
- Purity:
- 99.9%
- Supply Ability:
- 100 Tons Min