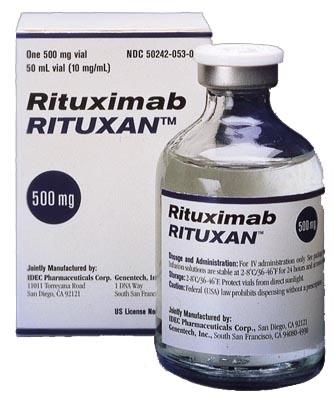
Several mechanisms of action of rituximab
Rituximab has become a mainstay in treating a broad variety of B-cell malignancies. In some B-cell malignancies, rituximab alone can induce high response rates and long-term remissions, while in others, adding rituximab to chemotherapy enhances the rates of complete response, long-term remission, and cure. Despite its undeniable value as a component of therapy for B-cell malignancies, rituximab is not effective for all patients, and the development of resistance to therapy is common. Understanding the mechanisms by which rituximab induces anti-tumor responses is central to our ability to improve on what is already a highly effective therapy.

While rituximab has been used in various indications, except lymphoma, where the target lymphoma cells are eliminated by rituximab, it is not entirely clear that rituximab was responsible for the improvement seen since multiple agents had been used in combination. If one allows the positive results to be seen because of rituximab and not in spite of it, then the mechanism must be established. There are three potential, and not necessarily mutually exclusive, mechanisms:
First, rituximab may be acting as a nonspecific intravenous immunoglobulin (IvIg). While the clinically used dose might seem too low to see an effect, recent data suggest that IvIg and a commercially available humanized monoclonal antibody were able to inhibit anaphylatoxin-C3a and -C5a-induced calcium responses in vitro and to block cellular migration and lethal C5a-mediated circulatory effects in vivo in mice and pigs at a concentration of 10 mg/mL, a concentration easily surpassed at the peak of a rituximab infusion.
Second, rituximab may deplete specific anti-donor antibodies. In the study of nine sensitized dialysis patients treated with single doses of rituximab, there was no appreciable change in PRA 2/9 (22%). Among the other seven, one had a decrease in PRA from 87% to 51% with a concurrent decrease in fluorescence intensity; five had changes in histogram architecture suggesting loss of antibody specificity; one subject had a four-fold decrease in PRA titer from 1:64 to 1:16 at 6 months after treatment. In addition, one of the seven converted a living kidney donor, donor-specific crossmatch to negative, and underwent a successful kidney transplant from that donor. In a more detailed analysis using single antigen beads, researchers found that specificities with lower titers were more likely to fall after rituximab treatment. Such an effect is not, however, likely as an explanation of the reported efficacy in the treatment of rejection because of the relatively rapid response noted in those patients treated with rituximab. With a half-life of 21 days, to eliminate 99% of circulating specific antibodies would require at least 4 months, and this only if antibody production completely and immediately ceased with rituximab. Since antibodies are made primarily by plasma cells that have a minimal expression of CD20 and are not eliminated by rituximab, such a mechanism is further questioned. A debate in the literature exists about whether plasma cells are long or shortlived. If the former, some method to deplete plasma cells might be needed. If the latter, then as CD27+ memory B cells are eliminated, and no source of alloantigen is present to re-stimulate newly appearing ¨ıve B cells. The alloantibody titer and PRA should fall over time at a rate controlled by the half-life of immunoglobulin and the half-life of plasma cells.
Third, rituximab may act by eliminating B cells. B cells are very efficient antigen-presenting cells, particularly after activating them. Such activation could occur at the time of rejection. The rapidity with which rituximab eliminates circulating and presumably tissue CD20+ B cells is consistent with this mechanism of action. The control of the rejection would occur because of loss of antigen presentation, resulting in less stimulation of T cells. However, it could include the elimination of B-cell-produced cytokines that are either directly damaging to the organ or that stimulate or recruit other cells that are damaging. Supporting the direct role of B cells in rejection is the report of Sarwal et al. showing that CD20 gene expression was associated with a worse prognosis. More recently, Hippen et al. showed that subjects with CD20-positive rejection had worse long-term renal graft survival. Of 27 patients with biopsy-proven Banff 1-A or Banff 1-B rejection in the first year after transplantation, 6 had CD20-positive B-cell clusters in the interstitium, and 21 did not. The CD20-positive group had reduced graft survival compared to CD20-negative controls. Treatment with rituximab of a patient with such CD20 cells in the biopsy and rejection resistant to steroids and anti-thymocyte globulin was successful.
References
[1] Pescovitz, M.D. “Rituximab, an Anti-CD20 Monoclonal Antibody: History and Mechanism of Action.” American Journal of Transplantation 6 5 (2006): Pages 859-866.
[2] Weiner, George J. “Rituximab: Mechanism of Action.” Seminars in hematology 47 2 (2010): Pages 115-123.
Related articles And Qustion
See also
Lastest Price from Rituximab manufacturers
US $0.00/G2025-04-21
- CAS:
- 174722-31-7
- Min. Order:
- 1G
- Purity:
- 98%min
- Supply Ability:
- 30kg/month
US $1.10/g2021-07-02
- CAS:
- 174722-31-7
- Min. Order:
- 1g
- Purity:
- 99.9%
- Supply Ability:
- 100 Tons Min