Depolarising neuromuscular blocking agent - Suxamethonium (succinylcholine chloride)
This quaternary ammonium compound is comparable to two molecules of acetylcholine linked together (Fig. 1). The two quaternary ammonium radicals, N+(CH3)3, have the capacity to cling to each of the α units of the postsynaptic acetylcholine receptor, altering its structural conformation and opening the ion channel, but for a longer period than does a molecule of acetylcholine. Administration of suxamethonium therefore results in an initial depolarisation and muscle contraction, termed fasciculation. As this effect persists, however, further action potentials cannot pass down the ion channels, and the muscle becomes flaccid; repolarisation does not occur.
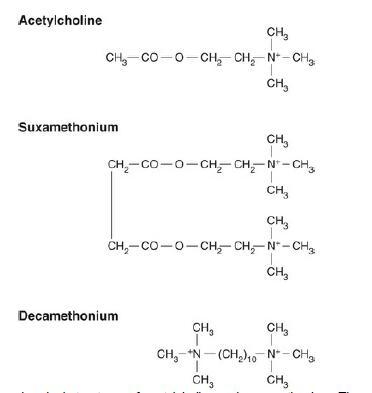
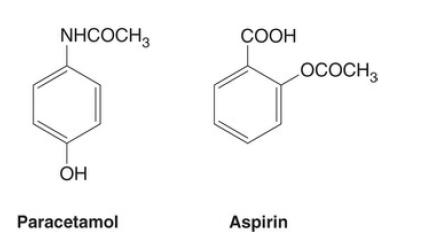
FIG. 1 The chemical structures of acetylcholine and suxamethonium. The
similarity between the structure of suxamethonium and two molecules of
acetylcholine can be seen. The structure of decamethonium is also shown. The
quaternary ammonium radicals N+(CH3)3 cling to the α subunits of the postsynaptic
receptor.
The dose of suxamethonium necessary for tracheal intubation in adults is 1.0–1.5 mg kg–1. This dose has the most rapid and reliable onset of action of any of the N MBA s presently available, producing profound block within 1min. Suxamethonium is therefore of particular benefit when it is essential to achieve tracheal intubation rapidly, such as in a patient with a full stomach or an obstetric patient.
The drug is metabolised predominantly in the plasma by the enzyme plasma cholinesterase, at one time termed pseudocholinesterase, at a very rapid rate. Recovery from neuromuscular block may start to occur within 3min and is complete within 12–15min. The use of an anticholinesterase such as neostigmine, which would inhibit such enzyme activity, is contraindicated. A bout 10% of the drug is excreted in the urine; there is very lile metabolism in the liver, although some breakdown by nonspecific esterases occurs in the plasma.
If plasma cholinesterase is structurally abnormal because of inherited factors, or if its concentration is reduced by acquired factors, then the duration of action of the drug may be altered significantly.
Adverse effects of suxamethonium
Although suxamethonium is a very useful drug for achieving tracheal intubation rapidly, it has several undesirable effects which may limit its use.
Muscle pains
Muscle pains occur especially in the patient who is ambulant soon after surgery, such as the day-case patient. The pains, thought possibly to be caused by the initial fasciculations, are more common in young, healthy patients with a large muscle mass. They occur in unusual sites, such as the diaphragm and between the scapulae, and are not relieved easily by conventional analgesics. The incidence and severity may be reduced by the use of a small dose of a non-depolarising NMBA given immediately before administration of suxamethonium (e.g. atracurium 0.05mgkg-1). However, this technique, termed precurarisation or pretreatment, reduces the potency of suxamethonium, necessitating administration of a larger dose to produce the same effect. Between 1 and 3min have been recommended between administering the non-depolarising NMBA and the subsequent suxamethonium, which can lead to a period of partial curarisation in an awake patient. Many other drugs have been used in an attempt to reduce the muscle pains, including lidocaine, calcium, magnesium and repeated doses of thiopental, but none is completely reliable.
Increased intraocular pressure
Increased intraocular pressure is thought to be caused partly by the initial contraction of the external ocular muscles and contracture of the internal ocular muscles after administration of suxamethonium. It is not reduced by precurarisation. The effect lasts for as long as the neuromuscular block, and concern has been expressed that it may be sufficient to cause expulsion of the vitreal contents in the patient with an open eye injury. This is unlikely. Protection of the airway from gastric contents must take priority in the patient with a full stomach in addition to an eye injury, as inhalation of gastric contents may threaten life. It is also possible that suxamethonium may increase intracranial pressure, although this is less certain.
Increased intragastric pressure
In the presence of a normal lower oesophageal sphincter, the increase in intragastric pressure produced by suxamethonium should be insufficient to produce regurgitation of gastric contents. However, in the patient with incompetence of this sphincter from, for example, hiatus hernia, regurgitation may occur.
Hyperkalaemia
It has long been recognised that administration of suxamethonium during halothane anaesthesia increases serum potassium concentration by 0.5mmol l–1. This is thought to be caused by muscle fasciculation. It is probable that the effect is less marked with the newer potent inhalational agents isoflurane, sevoflurane and desflurane. A similar increase occurs in patients with renal failure, but as these patients may already have an elevated serum potassium concentration, such an increase may precipitate cardiac irregularities and even cardiac arrest.
In some conditions in which the muscle cells are swollen or damaged, or in which there is proliferation of extrajunctional receptors (see Table 8.1), this release of potassium may be exaggerated. This is most marked in the burned patient, in whom K+ concentrations up to 13mmol l –1 have been reported. Suxamethonium should be avoided in this condition. I n diseases of the muscle cell or its nerve supply, hyperkalaemia after suxamethonium may also be exaggerated. These include the muscular dystrophies, dystrophia myotonica and paraplegia. Hyperkalaemia has been reported to cause death in such patients. S uxamethonium may also precipitate prolonged contracture of the masseter muscles in patients with these disorders, making tracheal intubation impossible. The drug should be avoided in any patient with a neuromuscular disorder, including the patient with malignant hyperthermia, in whom the drug is a recognised trigger factor.
Hyperkalaemia after suxamethonium has also been reported, albeit rarely, in patients with widespread intra-abdominal infection, severe trauma and closed head injury.
Cardiovascular effects
Suxamethonium has muscarinic, in addition to nicotinic, effects, as does acetylcholine. The direct vagal effect (muscarinic) produces sinus bradycardia, especially in patients with high vagal tone, such as children and the physically fit. It is also more common in the patient who has not received an anticholinergic agent (such as glycopyrronium bromide) or who is given repeated increments of suxamethonium. It is advisable to use an anticholinergic routinely if it is planned to administer more than one dose of suxamethonium. Nodal or ventricular escape beats may develop in extreme circumstances.
Allergic anaphylaxis
Immunoglobulin E (IgE)–mediated allergic reactions to suxamethonium are rare but may occur, especially after repeated exposure to the drug. They are more common after suxamethonium than any other neuromuscular blocking agent. A blood test is available to measure plasma suxamethonium IgE concentrations to aid in the diagnosis of allergic anaphylaxis to this agent. No such test is available commercially for the other NMBAs.