Testosterone: Effects on Lipids and Metabolic Mechanisms
Testosterone (T) is a predominantly male hormone responsible for virilization of the external male genitalia during embryonic development, promotion of somatic growth and secondary sexual characteristics in puberty, normal sexual function and libido in both males and females and promotion of bone formation, bone health and maintenance of bone and muscle mass in adults. It circulates in females at approximately 13-14% of the level observed in males. Testosterone levels in females decrease from approximately 20 years to 40 years of age and start rising again between 38 and 50 years old, but never reach the 20 years old.

The different concentrations of gonadal hormones in men and women are thought to be important factors contributing to the sex difference in lipoprotein profiles. Epidemiological data suggest that T levels are negatively associated with total cholesterol, LDL-C, and triglyceride (TG), while in men, T levels appear to have a complicated and controversial relationship with HDL-C levels and cardiovascular risk. In fact, androgen levels within the average adult male range were found to have a suppressive effect on HDL-C. On the other hand, several studies on patients with coronary artery disease have shown that higher T levels are associated with higher HDL-C concentrations. In particular, it was found that two genes involved in the catabolism of HDL-C are upregulated by T, namely, hepatic lipase (HL) and scavenger receptor B1 (SR-B1). SR-B1 mediates the selective uptake of HDL-C lipids into hepatocytes and steroidogenic cells, including Sertoli and Leydig cells of the testes, as well as cholesterol efflux from peripheral cells. T upregulates SR-B1 in the human hepatocyte and in macrophages and thereby stimulates selective cholesterol uptake and cholesterol efflux, respectively. HL hydrolyzes phospholipids on the surface of HDL-C, facilitating the selective uptake of HDL-C lipids by SR-B1. The activity of HL is increased after administration of exogenous T. The increases in SR-B1 and HL activities are consistent with the total cholesterol-lowering effect of T.
The mechanisms linking testosterone with insulin resistance and T2DM are still not fully understood. There are few published papers that have investigated potential mechanisms by which testosterone increases insulin sensitivity and regulates glucose and lipid metabolism. The primary insulin-responsive target tissues, such as skeletal muscle, liver and adipose tissue, inadequately respond to the physiologic effects of circulating insulin in T2DM. Impaired insulin sensitivity in these three tissues is characterized by defects in insulin-stimulated glucose transport activity, in particular into skeletal muscle, impaired insulin-mediated inhibition of hepatic glucose production and stimulation of glycogen synthesis in the liver, and a reduced ability of insulin to inhibit lipolysis in adipose tissue. In addition, as a consequence of dissociated fatty acid (FA) release from adipose tissue surplus to energy requirements in other organs, fat deposition in nonadipose tissue, including skeletal muscle and liver, occurs as a ‘spillover’ effect. In turn, this lipid accumulation contributes to impaired insulin responsiveness and abnormalities in glucose control. Indeed, fat in the liver and muscle correlates more strongly with insulin sensitivity than abdominal fat in rats. A growing body of studies has pointed to the presence of heterogeneity regarding insulin resistance and insulin sensitivity among different tissues; therefore, the mechanisms by which testosterone may impart beneficial actions on the development of T2DM and MetS are likely to be tissue-dependent and involve multiple targets of lipid and carbohydrate metabolism.
Testosterone deficiency is associated with decreased lean body mass, and relative muscle mass is inversely associated with insulin resistance and pre-diabetes. As up to 70% of the body’s insulin sensitivity is accounted for by muscle, low testosterone may lead to insulin resistance via anabolic and/or metabolic effects on muscle.
Muscle tissue additionally plays a role in lipid metabolism. Fat is oxidized in the liver and extra-hepatic tissue, such as skeletal muscle, and testosterone may influence this component of lipid metabolism.
It has long been known that castration is followed by decreased muscle glycogen levels in rat perineal and levator ani muscles and that administering testosterone induces a considerable increase in glycogen content. An equal increase in skeletal muscle glycogen synthesis is apparent in castrated male rats supplemented with testosterone, diminishing the elevated blood glucose levels seen in untreated controls. A testosterone-induced increase in glycogen synthase activity was implicated in the alteration in the rate of glycogen synthesis from blood glucose. Concurrently, testosterone administration returned the enhanced glycogen phosphorylase activity in castrated rats to an average level, thus reducing glycogen breakdown and the subsequent rise in free glucose. By contrast, the rate of glycogenesis was shown to be depressed by testosterone in rat skeletal muscle with increased glycogen content postulated rather than as a result of decreased glycogenolysis. In perineal muscle, however, glycogenesis was increased in response to testosterone, suggesting differential mechanisms in different tissue locations.
References:
[1] STELLA VODO. Testosterone-induced effects on lipids and inflammation.[J]. ACS Applied Energy Materials, 2013. DOI:10.1155/2013/183041.[2] DANIEL M KELLY T H J. Testosterone: a metabolic hormone in health and disease.[J]. Journal of Endocrinology, 2013, 217 3. DOI:10.1530/JOE-12-0455.
Related articles And Qustion
Lastest Price from Testosterone manufacturers

US $600.00/kg2025-11-24
- CAS:
- 58-22-0
- Min. Order:
- 1kg
- Purity:
- 99
- Supply Ability:
- 999

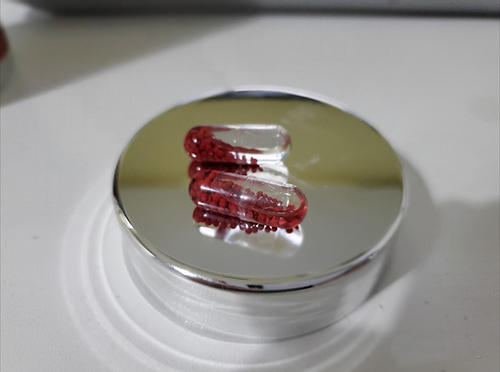
US $10.00/box2025-10-12
- CAS:
- 58-22-0
- Min. Order:
- 1box
- Purity:
- 99.99%
- Supply Ability:
- 9999