Pharmacology of Etomidate
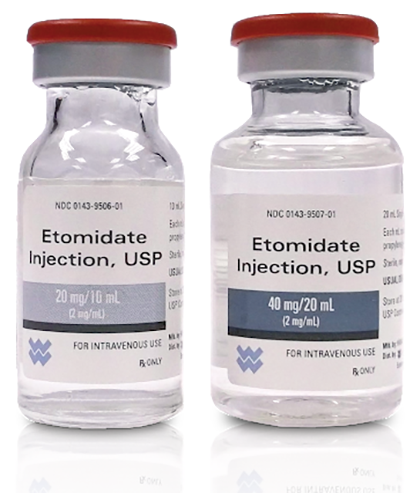
Etomidate, a carboxylated imidazole compound, was introduced in 1972. Etomidate is soluble but unstable in water. It is typically presented as the active R(+) enantiomer dissolved in propylene glycol or as a lipid emulsion containing medium-chain triglycerides. Ampoules contain 2mgml −1 etomidate in 10 ml.
Pharmacology
Etomidate is a rapidly-acting general anaesthetic agent with a short duration of action. It produces less cardiovascular depression than propofol in healthy patients, but this benefit is limited if the cardiovascular system is compromised (e.g. by severe hypovolaemia). Large doses may produce tachycardia. Respiratory depression is less than with other agents.
Pharmacokinetics
Etomidate redistributes rapidly in the body, and rapid elimination also occurs. It is metabolised in the plasma and liver, mainly by ester hydrolysis, and the metabolites are excreted in the urine; 2% is excreted unchanged. The terminal elimination half-life is 2.4–5h. There is little accumulation when repeated doses are given. The distribution and clearance of etomidate may be altered by concomitant administration of synthetic opioids. Metabolism is inhibited by fentanyl.
Adverse effects
Adverse effects include the following:
• Suppression of adrenal enzymes. Etomidate impairs adrenal cortisol synthesis by inhibition of the enzyme 11β-hydroxylase and response to adrenocorticotrophic hormone (ACTH). This effect occurs after a single bolus and lasts for several hours. At much higher doses, other enzymes such as 18β-hydroxylase are inhibited, reducing aldosterone and other steroid hormone synthesis. Long-term infusions of the drug in intensive care are associated with increased infection and mortality, probably related to impaired immunological competence.
• Venous thrombosis. This is more common than with other agents if the glycol preparation (Hypnomidate) is used.
Specific indications
Outpatient anaesthesia
Etomidate may be suitable in this situation, but the incidence of excitatory phenomena is unacceptably high unless combined with a benzodiazepine/opioid.
Compromised cardiovascular status
Depression is minimal with etomidate compared with other agents. However, etomidate should be avoided in patients who are expected to require level 3 intensive care postoperatively (e.g. after surgery for sepsis) because it causes adrenal suppression.