Application of Etomidate
Background
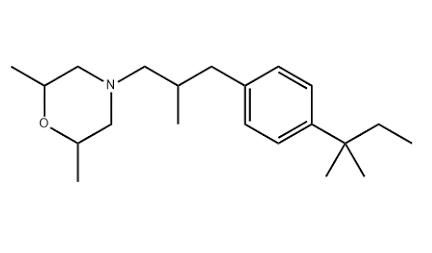
Etomidate, main function, induction of general anesthesia (short-term anesthesia must be combined with analgesics[1]. White powder, density: 1.11g/cm3, melting point: 72-74ºC, refractive index: 1.561, storage condition: 2-8ºC. Etomidate is a hypnotic intravenous general anesthetic, an imidazole derivative with high safety. It is one of the commonly used drugs for anesthesia induction, and etomidate has been used clinically for 30 years. Etomidate is a non-barbiturate intravenous sedative drug, which is a hydroxylated salt of imidazole. Its structural formula is shown in the following figure, the molecular formula is C14H16N2O2, and the molecular weight is 244.29. Etomidate is insoluble in water and unstable in neutral solutions.
Picture 1 Etomidate injection
Dosage form for clinical application
There are two main dosage forms in clinical application: ① water preparation: an injection prepared by dissolving etomidate in 35% propylene glycol; ② fat emulsion: prepared by dissolving etomidate in 20% medium and long chain triglycerides into the injection. In addition to the main solvent, the main difference between the two dosage forms is the osmotic concentration. The osmotic concentration of the water preparation is 4640mOsm/L, which is much higher than the physiological osmotic concentration; the osmotic concentration of the emulsion is 390 mOsm/L, which is close to the physiological osmotic concentration range. Therefore, compared with water preparations, fat emulsions can significantly reduce side effects such as injection pain and vascular damage. No precipitation occurs when etomidate is mixed with commonly used clinical anesthesia drugs such as muscle relaxants, vasoactive drugs or lidocaine. Etomidate injection should be stored at 2°C to 25°C and should not be frozen.
Pharmacokinetics
Distribution and binding After intravenous injection, etomidate quickly enters the brain and other organs with rich blood perfusion, followed by tissues and organs with slower uptake such as muscle and adipose tissue, and its distribution conforms to the three-compartment open model[2]. The initial distribution half-life of etomidate is 2.7 min, the redistribution half-life is 29 min, and the elimination half-life is 2.9-5.3 h. The onset time of a single intravenous injection of etomidate is related to the initial distribution half-life, usually within 30 to 60 seconds. The steady-state volume of distribution of etomidate was 2.2 to 4.5. 76.5% of etomidate was bound to plasma proteins (mainly albumin bound, 0.3 mg/kg single injection of etomidate for the time course of plasma clearance).
Metabolism and excretion Etomidate can be rapidly hydrolyzed by esterases in the liver and plasma and lose its activity. Its main metabolite is carboxylic acid. Only 2% of the drug is excreted in its original form, and the rest is excreted from the kidneys in the form of metabolites (85%). ) and bile (13%) excretion. The liver clearance rate is very high, reaching 18~25ml/(kg.min), and the liver uptake rate is 0.5~0.9.
Pharmacodynamics
Cardiovascular system: Etomidate has little effect on cardiovascular function. Under the clinical routine dose, the heart rate, mean arterial pressure, mean pulmonary artery pressure, pulmonary capillary wedge pressure, central venous pressure, cardiac stroke volume, cardiac index, pulmonary vascular resistance and peripheral vascular resistance are almost no Variety.
The hemodynamic stability of etomidate is related to its lack of effect on baroreceptor function, no effect on peripheral vasomotor function and no inhibition of myocardial contractility.
Central nervous system: Etomidate has central sedative, hypnotic and amnestic effects, but has no analgesic and muscle relaxant effects. The pharmacological effects of etomidate are mainly related to GABAA receptors. The relationship between hypnotic effects and β2 and β3 subunits of GABAA receptors is greater than that of α1 subunits. GABAA receptor antagonists can antagonize their effects. The plasma drug concentration required for etomidate anesthesia maintenance is about 300-500, 150-300 for sedation, and awakening when the plasma drug concentration drops to about 150-250.
A single intravenous injection of 0.2-0.3 etomidate reduced cerebral blood flow by 34% without affecting mean arterial pressure, but decreased cerebral oxygen metabolism rate (CMRO2) by 45%. Therefore, the cerebral oxygen supply and demand ratio increased significantly. In addition, etomidate can significantly decrease intracranial pressure with increasing dose, so etomidate is beneficial to maintain cerebral perfusion pressure. Because etomidate can reduce cerebral oxygen metabolism rate and intracranial pressure, it has a certain cerebral protective effect.
Respiratory system: Etomidate has little effect on the respiratory system, including spontaneous breathing, ventilation, and airway responsiveness. Therefore, the application of etomidate to maintain spontaneous breathing has obvious advantages, and no histamine release was observed even when etomidate was administered to patients with airway hyperresponsiveness. Others The therapeutic index (LD50/ED50) of etomidate is 26.4, and the safe dose range is wide.
Instructions
The pharmacological characteristics of etomidate are an important basis and basis for clinical application: etomidate has sedative, hypnotic and amnestic effects, but has no analgesic and muscle relaxant effects, and is an important sedative in general anesthetic drug combinations; etomidate Ester has a rapid onset of action, rapid metabolism and clearance in the body, and CSHT studies have shown that there is no significant accumulation in the body after continuous infusion; etomidate's slight inhibition of circulation is its outstanding advantage. The metabolic rate can also reduce intracranial pressure without affecting cerebral perfusion pressure. Etomidate emulsion can significantly reduce adverse reactions such as injection pain and vascular injury, all of which provide a good background for clinical application.
Reference
1 Liu Ji, Li Jinbao, Deng Xiaoming. Feasibility study of target-controlled infusion of etomidate for maintenance of general anesthesia. 2009
2 Liao Chaohui, Xing Biao, Shen Xianwen, etc. The effect of midazolam and fentanyl on myoclonus induced by etomidate. 2010