Exposure Sources & Medical Management of Beryllium
Target organ(s): Lung, skin, mucosal membranes
Occupational exposure limits: OSHA PEL: 2 μg/m3, TWA. Ceiling: 5 μg/m3 STEL (30 min maximum): 25 μg/m3;
ACGIH: TLV–TWA: 0.05 μg/m3; NIOSH TWA–REL: 0.5 μg/m3
EPA (air emissions): 10 g/24 h Reference values: EPA IRIS: Rfd: 2 × 10
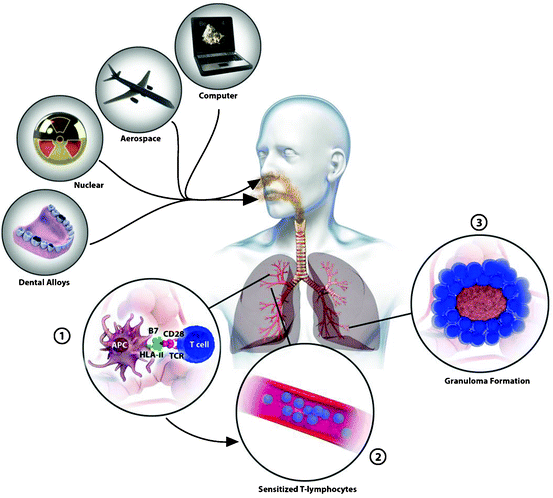
SOURCES OF EXPOSURE
Occupational
Increases and improvements in engineering controls have reduced the nature and degree of employee occupational exposure. However, normal industrial operations coupled with accidental releases do allow for exposures of varying concentrations and types.
Occupational overexposure to beryllium occurs primarily via the inhalation route, although dermal exposure from particulate dust is also a consideration. Occupationallyrelated ingestion is rare with adequate engineering controls, although it can occur from respiratory clearance mechanisms allowing particulate-embedded mucus to be swallowed. Overexposure can occur during the processing of alloys and ceramics and from the generation of dusts, fumes, and other fine particulates during the manufacture of berylliumcontaining materials.
Beryllium sensitization and CBD rates are clearly associated with the nature of the industry and the work process associated with the employee exposure. Newman et al. (2005) found that machinists were most likely to progress fromBeS to CBD than other workers within the same industry. Stanton et al. (2006) found that BeS andCBDrates in the employees of beryllium-processing plants exceeded workers handling manufactured products, such as in a beryllium–copper alloy distribution center.
There is also substantial evidence that the form of beryllium exposure is directly related to its ability to induce sensitization; not all beryllium is equivalent and not all beryllium is capable of inducing disease. Deubner et al. (2001) examined 75 workers at a beryllium ore mining and milling facility in Utah. The workers involved in the mining operation were primarily exposed to beryl ore or bertrandite ore, and the milling operation workers were exposed to these ores and beryllium hydroxide. General area, breathing zone, and personal lapel samples were used to estimate the historical beryllium exposure. The mean general area, breathing zones, and personal lapel samples ranges were 0.3–1.1, 1.1–8.1, and 0.05–6.9 μg/ m3, respectively. No cases of BeS or CBD were found in workers who only worked in the mines, leading the study authors to suggest that the form of beryllium may influence the risk for developing BeS or CBD. Stefaniak et al. (2008) suggested that the difference in particle size between ore dusts and manufacturing dusts may account for a difference in bioavailability, subsequently affecting the alveolar particulate loads.
Aluminum production can be a cause of occupational beryllium exposure as beryllium is found in the bauxite ore mined for aluminum. Taiwo et al. (2010) found a prevalence of 0.47% of BeS in a composite study of nine aluminumsmelting plants located throughout four countries and speculated that the lower sensitization rate may be “related to work practices and the properties of the beryllium found in this work environment.”
Biomonitoring of berylliumexposures have been attempted through urine samples, but no correlation between ambient air concentration and urinary levels has yet been identified. Apostoli and Schaller (2001) in a study of metallurgical workers did indicate higher levels of beryllium in “exposed” workers versus controls. They stated, however, that their study had too limited a dataset to make exact correlations “without reservations.” To date, there are no biological exposure indices (BEI) for beryllium urinary levels.
Environmental
The average amount of beryllium permeating the earth’s crust is roughly 6 mg/kg—calculated from the beryllium ore content in soils as elemental beryllium is too reactive to occur naturally. Natural sources of beryllium in ambient air come from natural rock erosion, volcanic dusts, and combustion ash. Major manmade ambient air sources are manufacturing and processing of ores and from the combustion of coals as they are commonly combustion agents in power plants for the production of electricity. Be concentration in coal averages 2.3 parts per million (ppm) and can be released into the air as fly ash and other coal combustion products (Eskenazy, 2006). Urban and industrial population may experience slightly higher ambient beryllium exposures; Detroit, Michigan averaged ambient air concentrations of 0.02–0.2 ng/m3 from 1982 to 1992 while the yearly average concentration for the entire United States is below the detection limit of 0.03 ng/m3 (ATSDR, 2002).
Soil contamination is also a consideration in environmental exposures. Contaminated soils increase the potential for elevated ambient air levels from fine dust, and children are at increased risk as they are more likely to inhale or ingest contaminated soils by their propensity to play in dirt. By 2002 beryllium was identified as a contaminant in at least 535 of the 1,613 current or former National Priorities List (NPL) sites; however, the beryllium form at these sites are “almost entirely” in insoluble forms and thus less likely to be exposure threats (ATSDR, 2002).
One of the primary concerns from environmental intrusion by beryllium is the potential for bioaccumulation. Ishikawa et al. (2004) found “abnormally high” levels of Be in samples of ascidian liver which they speculated may have been due to ascidian feeding on Be-enriched plankton. However, no study has found evidence of bioaccumulation moving up the food chain and ATSDR (2002) stated that Be “does not bioconcentrate in aquatic organisms.” Furthermore, a 2008 study of Floridian ospreys that “have frequently been used as indicator species for contamination” showed no significant elevation in trace beryllium. Samples were consistently below 1 μg/g dry feather weight (Lounsbury-Billie et al., 2008).
INDUSTRIAL HYGIENE
The generally accepted time-weighted occupational exposure limit of 2.0 μg/m3 has been utilized for various federal regulatory agencies since 1949 (Ward et al., 1992). Currently, Occupational Safety and Health Administration (OSHA) still sets the legally enforceable time-weighted average (TWA)–permissible exposure limit (PEL) as 2.0 μg/m3 with a ceiling of 5.0 μg/m3 and a 30 min peak level of 25 μg/m3. However, in light of some studies challenging the protectiveness of these limits, some agencies have modified their recommendations for occupational exposure limits. The NIOSH currently recommends a more conservative limit of 0.5 μg/m3, and in 2009, American Conference of Governmental Industrial Hygienists (ACGIH) significantly lowered their threshold limit value (TLV) to 0.05 μg/m3, a 40-fold reduction (ACGIH, 2009).
In their discussion of literature justifying reduction, ACGIH referenced reports by Kelleher et al., (2001); Madl et al., (2007); Schuler et al., (2005); Rosenman et al., (2005); and Stanton et al., (2006). However, Madl et al. (2007) pointed out that “(f)urthermore, no berylliumsensitized and CBD workers were exposed to a median concentration >2 μg/m3, but approximately 50% of the beryllium-sensitized and CBD workers were exposed to a 95th percentile concentration greater than 2 μg/m3 when looking at supplemented data for only the highest exposed year.” They also noted that “(t)wenty-six of the 27 berylliumsensitized and CBD workers had at least a 10% probability of being exposed to beryllium concentrations exceeding 0.2 μg/ m3 during their career, and all cases had a greater than 5% probability of exceeding this level.”
Kelleher et al. (2001) noted problems in determining significant differences between cases and control and stated that “(m)achinist history remained the only significant variable,” which thus encompasses a potential for particulate size as a variable. However, Kelleher et al. (2001) used lifetime exposure calculations to compare cases and controls, which might mask any particular exceedance of PELs. In their graphic representation, they noted that “the median cumulative exposure to total beryllium (based on the median exposure estimate) was 2.6 mg/m3-years in cases compared with 1.2 mg/m3-years in controls,” which implies a preponderance of PEL exceedance.
Borak (2006) in discussing a perceived need for lower regulatory limits admits that some studies that attribute BeS and CBD to exposure levels below 2.0 μg/m3 may actually have problems in Be contamination creating exposures exceeding 2.0 μg/m3. Stanton et al. (2006) noted study problems in small sampling sizes and poor historical exposure data. Schuler et al. (2005) also considered the possibilities that exposures may have actually exceeded 2.0 μg/m3. Despite the limitations in these studies, it is obvious that there is a growing concern as to the protectiveness of the current OSHA standard of 2.0 μg/m3, and that a revision of the standard to a lower PEL might reasonably be expected in the coming years.
No matter the exposure limit, good employee management and common sense dictate adherence to sound engineering and housekeeping controls. Proper personal protective equipment should be utilized when airborne exposures range near recommended exposure limits, and apparel should be protective against dermal exposures, especially in areas most prone to the presence of particulate matter or fumes. A 4-year program of instituting building design changes, restricted zone access, and required respirator wear in one facility resulted in a fourfold decrease in employee sensitization rates (Bailey et al., 2010). Therefore tracking areas of potential beryllium exposures in the workplace is imperative. Table 9.1 contains a list of the approved sampling protocols for quantification of beryllium in air or dust.
MEDICAL MANAGEMENT
The symptoms of acute or chronic beryllium-related disease may mimic other illnesses; for this reason, identification of beryllium exposure is critical in diagnosing the disease. A history of beryllium exposure, combined with weight loss, a nonproductive cough, eye irritation, irritation of the skin and respiratory tract, or pain in the sternum, suggests ABD. Chest X-rays can be useful in identifying pulmonary involvement, but have limited usefulness in diagnosis as the radiographic appearance is non-specific for beryllium disease (Stange et al., 1996). Thin-section computed tomography (TSCS) is a more sensitive technique than normal chest radiography, but it is only practical for confirmation of diagnosis rather than as a screening tool (Maier, 2002).
Chronic beryllium disease may be more difficult to diagnose than ABD because it generally requires months to years after the initial beryllium exposure and may manifest long after such exposure had stopped. Chronic beryllium disease may be precipitated by stress, such as surgery, combat, pregnancy, or another illness. Initially, CBD is characterized by shortness of breath on exertion, weight loss, chest pain, and cough. Reduced pulmonary function and reductions in vital capacity, forced expiratory volume, and maximal midexpiratory flow are indicators of possible CBD. Abnormal BeLPT test results may be indicators of BeS (the precursor of CBD) and can differentiate between a differential diagnosis of sarcoidosis and CBD.
Beryllium can be measured in the urine or in various tissues. However, as is true with many other metals, beryllium levels may not correlate with the level or duration of exposure. Elevated levels of beryllium do indicate exposure sometime in the past, but the time since exposure cannot be estimated because of beryllium’s long half-life.
Currently, the treatment protocol for beryllium disease is cessation of beryllium exposure and immunosuppression/ anti-inflammatory treatment with corticosteroids (Sood, 2009). Palliative treatment with supplemental oxygen and respiratory therapy can be helpful, but as of this time there is no curative therapy for BeS or CBD.
REFERENCES
Eskenazy, G.M. (2006) Geochemistry of beryllium in Bulgarian coals. Int. J. Coal Geol. 66:305–315.
Finch, G.L., et al. (1996) Animal models of beryllium-induced lung disease. Environ. Health Perspect. 104(Suppl. 5):973–979.
Goldberg, A. (2006) Beryllium Manufacturing Processes, United States Department of Energy.
Gordon, T. and Bowser, D. (2003) Beryllium: genotoxicity and carcinogenicity. Mutat. Res. 533:99–105.
Grier, R.S., Hood, M.B., and Hoagland, M.B. (1949) Observations on the effects of beryllium on alkaline phosphatase. J. Biol. Chem. 180:289–298.
Hardy, H.L. (1965) Beryllium poisoning—lessons in control of man-made disease. N. Engl. J. Med. 273:1188–1199.