Dulaglutide: Pharmacodynamics, Mechanism of action, Toxicity
General description
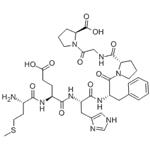
The Dulaglutide, with the CAS No: 923950-08-7, it is a novel, long-acting, glucagon-like peptide-1 (GLP-1) receptor agonist that has been developed by Eli Lilly and Company for the treatment of type 2 diabetes mellitus (T2DM). Dulaglutide is a once-weekly, GLP-1 receptor agonist, consisting of a DPP-IV-protected GLP-1 analogue covalently linked to a human IgG4-Fc heavy chain by a small peptide linker, thereby protecting the GLP-1 moiety from inactivation by dipeptidyl peptidase. In September 2014, the US FDA approved once-weekly subcutaneous dulaglutide, as an adjunct to diet and exercise, for the treatment of adult patients with type 2 diabetes mellitus. Dulaglutide 0.75 mg and 1.5 mg single dose pens have been to be available by the end of 2014. In the EU, the Committee for Medicinal Products for Human Use have recently recommended approval of subcutaneous dulaglutide in type 2 diabetes. Phase III/IIIb development of dulaglutide is also in progress in other countries worldwide, and the drug is under regulatory review in other countries.[1] This chemical’s molecular formula is C2646H4044N704O836S18 and molecular weight is 59 669.[2]
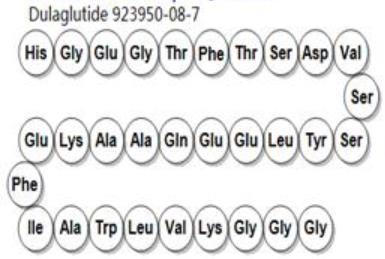
Figure 1 the molecular formula of Dulaglutide
Pharmacodynamics
Dulaglutide is a fusion protein produced using mammalian cell culture and consisting of two identical disulphidelinked chains, each with a N-terminal GLP-1 analogue sequence that is covalently linked by a peptide linker to the Fc component of a modified human immunoglobulin G4 heavy chain (IgG4 Fc). Fusion to this large carrier moiety slows its clearance from the body. The GLP-1 analogue component is 90 % homologous to endogenous human GLP-12, but with structural modifications in the area of the molecule that interacts with DPP-IV. Additional modifications were made in areas of the GLP-1 molecule that have potential as epitopes for T cells, and in areas of the IgG4 Fc component that bind Fc receptors and contribute to half-antibody formation. These modifications are intended to reduce the immunogenicity of the protein.[1,3]
The dulaglutide mechanism of action involves activation of the GLP-1 receptor, a membrane-bound cell-surface receptor coupled to adenylyl cyclase in b cells. Thus, it increases intracellular cyclic AMP in these cells, leading to a glucose-dependent release of insulin. Dulaglutide also reduces secretion of glucagon and slows gastric emptying. In clinical studies in patients with type 2 diabetes, onceweekly subcutaneous dulaglutide 0.75 or 1.5 mg reduced both fasting and postprandial serum glucose concentrations and postprandial serum glucose incremental area under the concentration-time curve (AUC) and increased first-and second-phase insulin secretion more than placebo. Compared with baseline, continued administration of dulaglutide increased fasting insulin and C-peptide concentrations and reduced fasting glucagon concentrations. In a thorough QTc study, there was no evidence of QTc prolongation at dulaglutide doses of 4 and 7 mg.[1]
Pharmacokinetics
Healthy adults and patients with type 2 diabetes have similar dulaglutide pharmacokinetics. Dulaglutide is slowly but well absorbed into the systemic circulation, reaching maximum plasma concentrations (Cmax)in 24–72 h (median 48 h) after a subcutaneous injection administered at steady state. With once-weekly injections, steady-state plasma concentrations were reached after 2–4 weeks. The site of the injection (abdomen, upper arm, thigh) had no statistically significant effect on dulaglutide systemic exposure. Following subcutaneous dulaglutide 0.75 and 1.5 mg, the mean absolute bioavailability values were 65 and 47 %, respectively; at corresponding doses, the mean volumes of distribution were 19.2 and 17.4 L.[1]It is assumed that dulaglutide is broken down into its component amino acids via pathways for general protein catabolism [1]. After administration of 0.75 or 1.5 mg doses, the elimination half-life for both doses was &5 days [1], which is consistent with once-weekly administration. There were no clinically important effects of age, sex, race, ethnicity or bodyweight on the dulaglutide Cmax or AUC; no dose adjustment is necessary based on these factors [1]. Similarly, there were no clinically important changes in the dulaglutide Cmax and AUC values in patients with mild, moderate or severe renal impairment (small increases were observed) or in patients with mild, moderate or severe hepatic impairment (small decreases were observed).[1]
Mechanism of action
The Dulaglutide is an incretin hormone that promotes glucose-dependent secretion of insulin from β cells and suppresses postprandial glucagon secretion from α cells, thereby supporting glucose homeostasis.[1]
Clinical efficacy
Most trials compare dulaglutide to placebo in addition to first-line metformin therapy and have demonstrated promising A1c reductions for dulaglutide. Grunberger et al completed a 12-week doubleblind, placebo-controlled study in 167 T2DM patients (A1c 7.2%±0.6%, duration of diabetes: 3.9 years) who had either received metformin therapy or were treatment naïve.[6] Patients were randomized to one of five treatment arms (placebo, 0.1 mg, 0.5 mg, 1 mg, or 1.5 mg dulaglutide) in a 1:1:1:1:1 manner with the primary endpoint being change from baseline A1c and secondary endpoints being efficacy and safety. Results demonstrated a dose-dependent A1c reduction (P,0.001 for all) for dulaglutide and greater reduction compared to placebo (P,0.001 for all) except for in the 0.1 mg dose. Similar results were seen for daily plasma glucose and fasting plasma glucose (FPG) with dose-dependent reductions for all (P,0.001) which were greater when compared to placebo (P,0.001) except for the 0.1 mg dose. More patients receiving dulaglutide achieved A1c reductions of #7% (P,0.001) or #6.5% (P,0.001) than those receiving placebo. Dose-dependent increases in the homeostasis model assessment (HOMA)2-B (a marker of basal beta-cell function to release insulin during the fasting state) were seen with all dulaglutide groups (P=0.036) and were greater than that for placebo except for the 0.1 mg dose (P#0.013); no changes were noted for any group for HOMA2-S (an assessment of insulin sensitivity). Body-weight reductions were noted for all dulaglutide groups with dose-dependent results; however, these were not significant when compared to placebo. Safety data showed treatment-emergent adverse drug events (ADEs) included nausea, diarrhea, and nasopharyngitis, with four patients discontinuing dulaglutide due to ADEs. Four cases of serious ADEs, with two of these linked to study drugs, included hemorrhagic pancreatitis associated with cholelithiasis (placebo) and abdominal pain/distension (dulaglutide 1.5 mg). No reports of severe hypoglycemia were noted, with rates of hypoglycemia similar across all groups. Both diastolic and systolic blood pressures were similar across all groups, along with levels of pancreatic enzymes being similar between groups at endpoint. One treatment-emergent case of anti-dulaglutide antibody (dulaglutide 1 mg) was reported, along with one patient reporting treatment-emergent skin rash and skin exfoliation (dulaglutide 0.1 mg).[5]
Toxicity
Adverse drug events of dulaglutide have been consistent with those of other agents in this class, with the most common seen being transient and mild GI side effects. These include nausea, vomiting, and diarrhea which are expected based upon the mechanism of action and usually decrease over time. Hypoglycemia is similar to other GLP-1 RAs and was typically not significant in the clinical trials, with no reports of severe hypoglycemia occurring in any trial. Injection-site reactions are also possible but have not been reported at a high rate in currently available clinical trials. Development of antibodies against the medication may potentially lead to reduced efficacy and/or changes in the safety profile. The risk with dulaglutide in clinical trials appears to be low according to currently available trials but varied from study to study from no reports to up to ten reports. Out of the reported cases, only one hypersensitivity reaction occurred resulting in treatment-emergent skin rash and skin exfoliation .Events were mostly mild to moderate and transient.[4,5]
References
[1]M Sanford. Dulaglutide:First Global Approval[J]. Drugs, 2014, 74 (17):2097-2103.
[2]Xu SS, Hua XY, Xiao L,et al. Dulaglutide: Novel, long-acting, glucagon-like peptide-1 (GLP-1) receptor agonist[J]. China Pharmacy, 2015, 26 (32):4593-4595.
[3]Glaesner W, Vick AM, Millican R, et al. Engineering and characterization of the long-acting glucagon-like peptide-1 analogue LY2189265, an Fc fusion protein. Diabetes Metab Res Rev. 2010, 26(4):287-296.
[4]Wysham C, Blevins T, Arakaki R, et al. Efficacy and safety of dulaglutide added onto pioglitazone and metformin versus exenatide in type 2 diabetes in a randomized controlled Trial (AWARD-1)[J]. Diabetes Care, 2014, 37(8):1393-1394.
[5] Krystal L , Edwards, Molly G , et al. Dulaglutide: an evidence-based review of its potential in the treatment of type 2 diabetes.[J]. Core evidence, 2015.
[6]Grunberger G, Chang A, Garcia Soria G, et al. Monotherapy with the once-weekly GLP-1 analogue dulaglutide for 12 weeks in patients with Type 2 diabetes: dose-dependent effects on glycaemic control in randomized, double-blind, placebocontrolled study. Diabet Med. 2012;29:1260-1267.
You may like
Related articles And Qustion
US $0.10/KG2025-09-15
- CAS:
- 923950-08-7
- Min. Order:
- 1KG
- Purity:
- 99.0%
- Supply Ability:
- 1000 tons

US $10.00-7.00/VIAL2025-07-24
- CAS:
- 923950-08-7
- Min. Order:
- 10VIAL
- Purity:
- 99.9
- Supply Ability:
- 20000