Curcumin as an Agent for Rapid Healing of Burns, and UV Light Injury and Photodamaged Skin
Types of Skin Injury
The ability of topical curcumin to assist in skin repair after injury may be a very important effect that
accounts for its widespread and longstanding popularity as a therapeutic cosmetic. The common types
of injury include surgical wounds, burns from heat (fires, heating pads, and scalds), laser burns, solarinduced
injury from UV radiation, and burns from ionizing radiation. The different types of wounds
vary with respect to their propensity to develop scarring, as well as a tendency for malignant transformation.
The pathways blocked by curcumin which may assist in skin repair with different types of injury
are discussed below.
Burns and Traumatic Wounds
Acute injury such as burns and scalds usually result in blister formation, swelling, and erythema, causing considerable pain to the patient, and resulting in loss of function. Excessive solar exposure causes acute sunburns, resulting in pain, erythema, and blistering. Sunburns are due to UV light injury mainly in the UVB spectrum (290–320 nm wavelength). Toxic chemicals cause “chemical burns,” damaging cytoplasmic proteins and releasing caspases from the mitochondria, and resulting in cellular necrosis or apoptosis. Laser-induced injury, which depends on the type of laser and wavelengths emitted by the instrument, usually resembles heat injury.
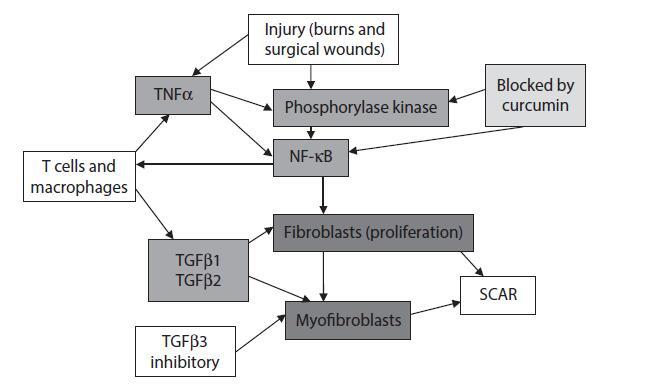
FIGURE 3.4 Signaling pathways in scar tissue formation after injury: targets for anti-scarring therapy by topical curcumin.
Burns and scalds are caused by heat injury to cellular proteins, resulting in coagulative necrosis of cells, and damage to cellular proteins within the cytoplasm and nucleus. Damage to DNA in the nucleus sets up the well-known DNA damage response (DDR) for repair of damaged DNA. However, the accompanying inhibition of cell proliferation (cell cycle arrest) associated with the DNA damage response impairs the ability of the cells to regenerate new cells, slowing down the repair process. Unlike wounds in embryos that usually heal without scarring, adult wounds almost always result in scarring. In contrast to embryonic tissue that do not usually express TGFβ1, the adult inflammatory process is associated with release of growth factors, in particular TGFβ1 (transforming growth factor-β1), especially after burns and scalds. This results in hypertrophic scar formation, which is commonly observed with second and third degree burns and scalds, with increasing scarring in deeper wounds. The formation of hypertrophic scars involves the conversion of fibroblasts to myofibroblasts, which is induced by secretion of excessive TGFβ1. Myofibroblasts possess contractile properties, which result in tissue induration characteristic of hypertrophic scarring and keloid formation. Increased TGFβ1 secretion is also noted in hypertrophic scars and keloids.
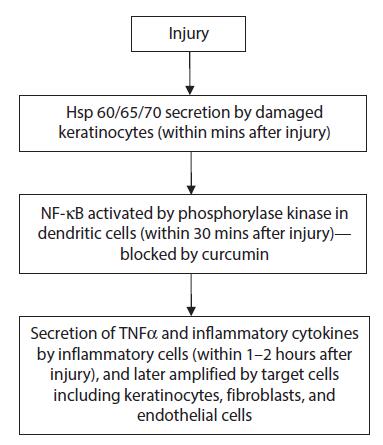
Injury to the skin results in signals leading to initiation of a cascade of events in the wound healing process. These include inflammation, neovascularization, scarring and epidermal proliferation, often with post-inflammatory hyperpigmentation or hypopigmentation. One of the earliest signaling events in the injury cascade involves the activation of the transcription activator NF-κB in dendritic cells, which are among the earliest inflammatory cells to respond to skin injury. By inhibiting PhK, which is activated within minutes following injury upstream of NF-κB, curcumin blocks NF-κB-induced signaling, with downstream reduction in inflammation and scar tissue formation from the inhibition of TGFβ1 secretion. This minimizes fibroblast proliferation and myofibroblast conversion. The key anti-scarring signaling pathways and targets blocked by curcumin are summarized in Figure 3.4. Topical curcumin has also been shown to heal burns with minimal scarring, and to achieve similar results in surgical wounds.
Curcumin as an Agent for Rapid Healing of Burns, and UV Light Injury and Photodamaged Skin
The wavelengths in sunlight that produce sunburns are usually attributed to those in the UV range, i.e., UVB (290–320 nm wavelength) and UVA (320–400 nm wavelength). Although UVB wavelengths are more prone to cause sunburn, current evidence suggests that UVA radiation, which makes up 95% of the solar UV light reaching the Earth, may be the more damaging of the two in regard to photocarcinogenesis (basal cell carcinomas and melanomas) and photoaging (pigmentary changes, wrinkling, and solar elastoses). Additionally, other wavelengths, such as infrared rays that produce heat, may also contribute to the injury observed in acute sunburns and chronic dermal injury.
Cyclobutane Pyrimidine Dimers and DNA Damage
Production of cellular point mutations and mutagenic cyclobutane pyrimidine dimers (CPD) has been shown with both UVB and UVA exposure. However, the CPDs produced by UVB tend to be easily removed and cause limited injury to the DNA. On the other hand, CPDs produced by UVA tend to be predominantly thymine–thymine pyrimidine dimers, which are located at the apex of the helical DNA strands, are difficult to remove, and tend to produce damage to large segments of the DNA. The damage induced by the large double-stranded DNA breaks are difficult to repair, and frequently result in errors of replication that cause normal cells to transform into their malignant counterparts. In addition, it has been observed that the “bystander effect,” in which tissue damage occurs outside the areas exposed to UV light, has only been observed with UVA radiation but not with UVB, accounting for many skin cancers and melanomas that develop in areas not exposed to solar radiation.
Signaling Pathways Induced by Acute and Chronic Solar Injury: Inhibition by Curcumin
Sunburn resembles other skin injuries in producing an inflammatory cascade that invokes the wound repair mechanism. The repair processes, resulting in the formation of new blood vessels and fibroblastic proliferation, frequently lead to dermal scarring. In addition, the skin damage results in epidermal and melanocytic proliferation, which are noted clinically as keratotic and pigmentary lesions. Repeated solar skin damage may lead to formation of premalignant solar lentigenes and dysplastic nevi. With chronic solar damage, DNA injury may result in photocarcinogenesis, with dysregulated cell cycling and malignant transformation. The above processes may lead to development of squamous cell and basal cell carcinomas, as well as malignant melanomas that can manifest clinically as lentigo maligna, superficial spreading melanomas, and nodular melanomas. The solar-induced injury pathways are mediated by NF-κB21-dependent signaling, and may potentially be inhibited by curcumin,as shown in Figure 3.5.
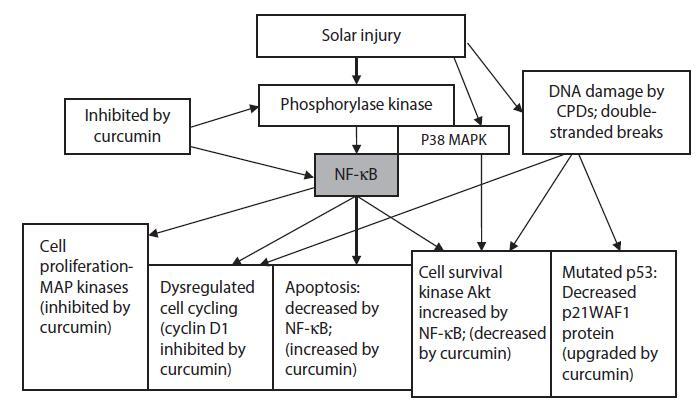
FIGURE 3.5 Signaling targets in acute and chronic solar injury inhibited by curcumin.
Besides the rapid heat shock protein-induced NF-κB activation mediated by Toll receptors, and MAP kinase signaling, another rapid-response cell survival pathway initiated by reactive oxygen species in response to UV irradiation in human keratinocytes has been identified, resulting in activation of pathways such as p38 MAP kinases and AKT, with activation of additional transcription activators. In cultured human keratinocytes, phosphorylation of p38 MAP kinase was initiated at 5 minutes, peaked at 30 minutes, and remained elevated up to 2 hours, while the phosphorylation of AKT started at 15 minutes, peaked at 1 hour, and remained elevated beyond 2 hours. It is likely that PhK, which is also activated within 5 minutes after injury, may also play a role in the phosphorylation of both p38 MAP kinase and AKT survival kinase. These alternative pathways synergize with the canonical pathways to amplify the immune response to injury. Using curcumin to block both the canonical and alternative pathways simultaneously has the advantage of synchronized mitigation of the amplified injury-induced inflammatory response. These mechanisms may be responsible for the anti-carcinogenic properties and reparative properties of curcumin reported clinically.
Laser and IPL Injury
While the severity of laser injury is dependent on the wavelength and intensity of the beam, laser damage to tissues appear to be similar to heat-induced injury.54–58 Skin injury occurs with more highly powered lasers. Laser beams and even broad spectrum radiation (intense pulsed light or IPL) ranging from the near UV visible spectrum to the infrared spectrum just below the microwave spectrum (400– 1400 nm) can produce damage by heat injury. Blistering and post-inflammatory hyperpigmentation has been observed with laser burns in the skin,54 with damage consistent with changes from heat-induced injury.
The sequence of inflammatory events following laser or IPL injury appears to be similar to those found with heat, UV light, and ionizing radiation. Within one hour following laser damage, dendritic cells, macrophages, and microglia were observed to migrate towards sites of injury. In patients with sun-damaged skin who received five monthly treatments, with one group receiving IPL and a second group receiving treatment with 1064 nm Nd:Yag laser, scattered dendritic cells expressing heat shock protein 70 were observed in the papillary and upper reticular dermis with both IPL and Nd:YAG laser treatments, and were associated with the expression of procollagen 1. These changes were seen in the post-treatment but not in the pre-treatment biopsies.
Increased risk of IPL-induced or laser-induced injury is observed with increasing doses, multiple treatments with short intervening periods, lack of cooling techniques, and the addition of other therapies such as photosensitizers in photodynamic therapy, including ala-aminolevulinic acid (Levulan). We have observed beneficial effects with the use of curcumin gel in injured skin from laser, IPL, and Levulan treatments (Heng MCY: unpublished data).
Summary
Phosphorylase kinase is a unique enzyme in which the spatial arrangements of the specificity determinants can be manipulated so that the enzyme can transfer high energy phosphate bonds to sites of differing specificities, such as serine, threonine, and tyrosine. Phosphorylase kinase may be involved in the early response mechanism that is responsible for the initiation and subsequent amplification of inflammation induced by multiple injurious stimuli. By synergistically augmenting ATP tissue supplies, and phosphorylating multiple serine/threonine and tyrosine specific sites, including those molecules required for transcription activation, phosphorylase kinase can affect multiple pathways involved in cytokine/ growth factor/chemokine-mediated inflammation involving cell proliferation, cell cycling, cell migration, inhibition of apoptosis, dysregulated cycling, and tumor transformation, with their attendant deleterious effects on injured tissues. By blocking these pathways with curcumin, a phosphorylase kinase inhibitor, it may be possible to mitigate these injury-triggered deleterious effects. Because of the poor bioavailability of oral curcumin, a topical curcumin preparation has been used to demonstrate the salutary effects of phosphorylase kinase inhibition in injured skin, in particular in the optimal healing of burns, surgical wounds, and photodamaged skin.
REFERENCES
1. Ohashi K, Burkhart V, Flohe S et al. Cutting edge: Heat shock protein 60 is a putative endogenous ligand
of the toll-like receptor-4 complex. J Immunol 2000;164:558–61.
2. Vabulas RM, Ahmad-Nejad P, da Costa C et al. Endocytosed HSP60s use toll-like receptor-2(TLR2) and
TLR4 to activate the toll/interleukin 1 receptor signaling pathways in innate immune cells. J Biol Chem
2001;276:31332–9.
3. Singh S, Aggarwal BB. Activation of transcription factor NF-kappa B is suppressed by curcumin (diferuloylmethane).
J Biol Chem 1995;270:24995–5000.
4. Bharti AC, Aggarwal BB. Nuclear factor-κB and cancer: Its role in prevention and therapy. Biochem
Pharmacol 2002;64:883–8.
5. Brash DE, Ziegler A, Jonsson AS et al. Sunlight and sunburn in human cancer: p53, apoptosis, and tumor
promotion. J Invest Dermatol 1996;1:136–42.
6. El Deiry WS, Tokina T, Vekulescu VE et al. WAF1, a potential mediator of p53 tumor suppression. Cell
1993;75:817–25.
7. Park MJ, Kim EH, Park IC et al. Curcumin inhibits cell cycle progression of immortalized human umbilical
vein endothelial (ECV304) cells by up-regulating cyclin-dependent kinase inhibitor, p21WAF1/CIP1,
p27KIP1 and p53. Int J Oncol 2002;21:379–83.
8. Takada Y, Singh S, Aggarwal BB. Identification of p65 peptide that selectively inhibits NF-kappa B activation
induced by various inflammatory stimuli and its role in down-regulation of NF-kappaB-mediated
gene expression and up-regulation of apoptosis. J Biol Chem 2004;279:15096–104.
9. Karin M, Ben-Neriah Y. Phosphorylation meets ubiquitination: The control of NF-[kappa]B activity.
Annu Rev Immunol 2000;18:621–63.
10. Palkowitsch L, Leidner J, Ghosh S et al. Phosphorylation of serine 68 in the IkappaB Kinase (IKK)-
binding domain of NEMO interferes with the structure of the IKK complex and tumor necrosis factoralpha-
induced NF-kappaB activity. J Biol Chem 2008;283:76–86.
You may like
Related articles And Qustion
Lastest Price from Curcumin manufacturers

US $1200.00-1100.00/ton2025-10-14
- CAS:
- 458-37-7
- Min. Order:
- 1ton
- Purity:
- 99%
- Supply Ability:
- 1000T/M

US $1200.00-1100.00/ton2025-09-25
- CAS:
- 458-37-7
- Min. Order:
- 1ton
- Purity:
- 99%
- Supply Ability:
- 1000T/M