Cobalt: Sources of Exposure & Medical Management
First aid (metal dust and fume): Eye: Irrigate immediately; skin: soap wash immediately; breathing: respiratory support; swallow: medical attention immediately.
Target organ(s): Respiratory tract, skin, heart, blood, thyroid gland, ear, eye
Occupational exposure limits: NIOSH REL: 0.05 mg/m3; OSHA PEL: 0.1 mg/m3; American Conference of Governmental Industrial Hygienists (ACGIH) TLV: Timeweighted average (TWA) 0.02 mg/m3; Cal/OSHA PEL: 0.02 mg/m3
Reference values: No reference dose or reference concentration set by EPA. Agency for Toxic Substances and Disease Registry (ATSDR) MRL: 0.0001 mg/m3 (inhalational), 0.01 mg/kg/day (ingestion); ATSDR MRL: 0.00003 mg/m3 (mice); CalEPA REL: 0.000005 mg/m3 (mice); NIOSH ILDH: 20 mg Co/m3
Risk phrases: 22-42/43
Harmful if swallowed
May cause sensitization by inhalation and skin contact
Safety phrases: 22-24-37
Do not breathe dust. Avoid contact with skin. Wear suitable gloves

SOURCES OF EXPOSURE
Occupational
Occupational exposure to cobalt occurs from diverse industries and occupations such as mining, heavy metal superalloy production, and tungsten carbide processing. In addition, workers are also exposed when cobalt or its compounds are involved in the refining of cobalt and processing of various alloys and its salts (Swennen et al., 1993). Cobalt air levels have been associated with corresponding incidence of occupational asthma and hard metal disease in the hard metal industry. Suspected asthma incidence was highest in powder plant maintenance, in areas of chemical testing, metal pressing, and sintering. Also, cases suspected of hard metal disease were observed in metal pressing, sintering, and grinding. Along with the respiratory route of occupational exposure, dermal exposure is also common. Exposure to cobalt is particularly common in workplaces that involve the use of cutting or grinding tools, refining or processing cobalt metal or ores, and ceramics. Exposure is also prevalent in industries using cobalt to color glass and producing drier for enamel and paint. For most of the cases, except in the processing of cobalt powder, the exposure is not only to cobalt but also to other metals and compounds like tungsten carbide, chromium, iron, etc. A combination of cobalt with these metals may alter the chemical reactivity of cobalt.
Environmental
Cobalt is found throughout the environment in low concentrations in air, food, and water. The amount of cobalt in air is <2 ng/m3, which is less than the cobalt exposure from food and water. In drinking water, cobalt concentration is <1–2parts per billion(ppb). An average person consumes about 11 μg of cobalt in the diet in the form of vitamin B12.
The concentration in food and water may be many times more in areas that are in the vicinity and/or in the areas of mining, smelting, or hard metal industries. Environmental exposure may occur from surgical procedures such as hip implants (Sunderman et al., 1989) and dental prosthesis (Kettelarij et al., 2014). Elevated blood cobalt levels were observed due to metal hip implants in the absence of other etiologies in patients undergoing total hip replacement (Pizon et al., 2013).
INDUSTRIAL HYGIENE
The Occupational Safety and Health Administration (OSHA) has assigned an 8-h permissible exposure limit (PEL) of 0.1 mg/m3, and the National Institute for Occupational Safety and Health (NIOSH) recommends an 8-h TWA of 0.05 mg/m3 (NIOSH, 2007). ACGIH has recommended an 8-h TWA of 0.02 mg/m3. No reference concentration (RfC) or reference dose (RfD) has been associated with cobalt and its compounds though ATSDR has recommended minimal risk levels (MRL) of 0.0001 mg/m3 via inhalational route and 0.01 mg/kg/day via ingestion (ATSDR, 2004).
MEDICAL MANAGEMENT
Diagnosis
The diagnosis of respiratory illness associated with cobalt is by the worker complaints, work history and signs detected from X-ray abnormalities, pulmonary function tests, Bronchoalveolar lavage and lung biopsy, to high resolution tomography scanning (Dunlop et al., 2005; Gotway et al., 2002). Signs may include dyspnea, shortness of breath, and expectoration; physical examination may reveal crackles. Chest X-ray generally presents with a reticulo-nodular pattern predominantly in the lower zones. Pulmonary function tests may show lowered diffusion capacity with restrictive pattern. Bronchial lavage can reveal multinucleate giant cells and elevation in eosinophil count and T-lymphocytes. Lung biopsy may show giant cell interstitial pneumonitis, fibrosing alveolitis, or inflammatory infiltrates. In another study, high resolution tomography scanning indicated large cystic spaces in mid and upper lungs, upper lobe reticulation, and traction bronchiectasis (Gotway et al., 2002).
Biomonitoring can be undertaken to assess exposure and determine the efficacy of health and safety procedure. Concentrations of cobalt and its compounds in blood and urine show a positively linear association with air concentration levels (Ichikawa et al., 1985). Workers exposed to cobalt may have higher IgA levels and lowered IgE levels (Bencko et al., 1986). In one study human leukocyte antigen residue was monitored to distinguish workers exposed to cobalt and those predisposed to develop hard metal disease (Potolicchio et al., 1997).
Treatment
Early diagnosis and treatment is important in the management of cases exposed to cobalt and cobalt compounds. Removal of the worker from the exposure to cobalt and its compounds is an important initial step in the treatment protocol. In a study, cobalt-exposed workers with the symptoms of cough and eczema showed recovery when the exposure was withdrawn. One worker who remained on the job developed lung nodules 2.5 years later. In another study, proper diagnosis of three patients and removal from cobalt exposure resulted in complete recovery for two; the third had some mild lingering effects (Anttila et al., 1986). A fourth patient in the same report was not diagnosed efficiently and developed lingering, severe respiratory effects.
Treatment of chronic effects should be symptomatic. Studies have shown the improvement in symptoms in hard metal disease patients with the administration of steroids (Nureki et al., 2013), but no clinical trials have been performed to confirm the effectiveness of such agents.
REFERENCES
Chachami, G., et al. (2004) Cobalt induces hypoxia-inducible factor-1alpha expression in airway smooth muscle cells by a reactive oxygen species- and PI3K-dependent mechanism. Am. J. Respir. Cell Mol. Biol. 31(5):544–551.
Coates, E.O. Jr. and Watson, J.H. (1973) Pathology of the lung in tungsten carbide workers using light and electron microscopy. J. Occup. Med. 15(3):280–286.
Costa, M., et al. (1982) Selective phagocytosis of crystalline metal sulfide particles and DNA strand breaks as a mechanism for the induction of cellular transformation. Cancer Res. 42(7):2757–2763.
Cross, D.P., et al. (2001) Mixtures of nickel and cobalt chlorides induce synergistic cytotoxic effects: implications for inhalation exposure modeling. Ann. Occup. Hyg. 45(5):409–418.
D’Adda, F., et al. (1994) Cardiac function study in hard metal workers. Sci. Total Environ. 150(1–3):179–186.
You may like
See also
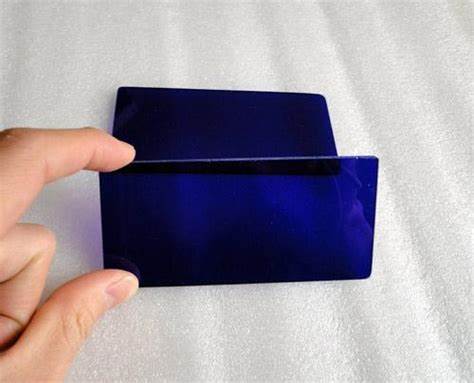
Lastest Price from Cobalt manufacturers

US $0.00-0.00/kg2025-12-13
- CAS:
- 7440-48-4
- Min. Order:
- 1kg
- Purity:
- 98%
- Supply Ability:
- 1000

US $6.00/kg2025-04-21
- CAS:
- 7440-48-4
- Min. Order:
- 1kg
- Purity:
- 99%
- Supply Ability:
- 2000KG/Month