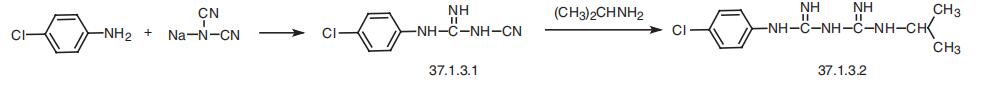
N-(4-CHLOROPHENYL)-N'-(ISOPROPYL)-IMIDODICARBONIMIDIC DIAMIDE
- Product NameN-(4-CHLOROPHENYL)-N'-(ISOPROPYL)-IMIDODICARBONIMIDIC DIAMIDE
- CAS500-92-5
- CBNumberCB7455742
- MFC11H16ClN5
- MW253.73
- EINECS207-915-6
- MDL NumberMFCD00866201
- MOL File500-92-5.mol
Chemical Properties
| Melting point | 129° |
| Boiling point | 399.65°C (rough estimate) |
| Density | 1.2039 (rough estimate) |
| refractive index | 1.6110 (estimate) |
| storage temp. | Store at -20°C, protect from light |
| solubility | DMF: 2mg/mL; DMSO: 3mg/mL; DMSO:PBS (pH 7.2) (1:10): 0.09mg/mL; Ethanol: 1mg/mL |
| form | A solid |
| pka | 11.15±0.10(Predicted) |
| color | White to off-white |
| FDA UNII | S61K3P7B2V |
| ATC code | P01BB01,P01BB51 |
Safety
| Symbol(GHS) |

|
|||||||||
| Signal word | Warning | |||||||||
| Hazard statements | H302-H315-H319-H335 | |||||||||
| Precautionary statements | P261-P280-P301+P312-P302+P352-P305+P351+P338 | |||||||||
| NFPA 704: |
|