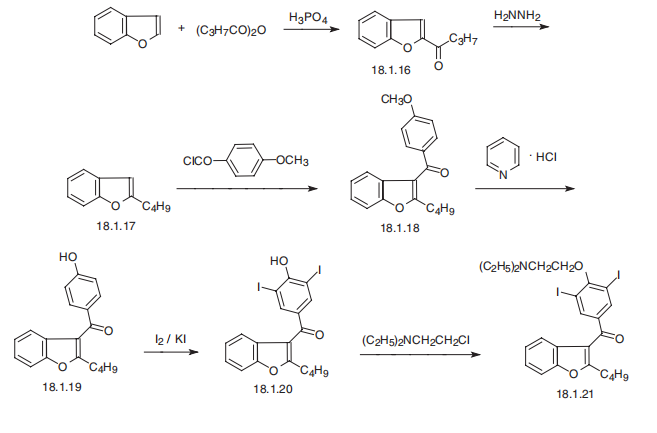
Amiodarone
- Product NameAmiodarone
- CAS1951-25-3
- CBNumberCB5310616
- MFC25H29I2NO3
- MW645.31
- EINECS217-772-1
- MDL NumberMFCD00242801
- MOL File1951-25-3.mol
- MSDS FileSDS
Chemical Properties
| Melting point | 54 - 55°C |
| Boiling point | 635.1±55.0 °C(Predicted) |
| Density | 1.5730 (estimate) |
| storage temp. | 2-8°C |
| solubility | Chloroform (Slightly), Methanol (Slightly) |
| form | Solid |
| pka | 6.56(at 25℃) |
| color | Colourless to Pale Yellow |
| Water Solubility | 716.4mg/L(25 ºC) |
| Stability | Stable. Incompatible with strong oxidizing agents. |
| InChI | InChI=1S/C25H29I2NO3/c1-4-7-11-22-23(18-10-8-9-12-21(18)31-22)24(29)17-15-19(26)25(20(27)16-17)30-14-13-28(5-2)6-3/h8-10,12,15-16H,4-7,11,13-14H2,1-3H3 |
| InChIKey | IYIKLHRQXLHMJQ-UHFFFAOYSA-N |
| SMILES | C(C1C2=CC=CC=C2OC=1CCCC)(C1=CC(I)=C(OCCN(CC)CC)C(I)=C1)=O |
| CAS DataBase Reference | 1951-25-3(CAS DataBase Reference) |
| FDA UNII | N3RQ532IUT |
| ATC code | C01BD01 |
| EPA Substance Registry System | Methanone, (2-butyl-3-benzofuranyl)[4-[2-(diethylamino)ethoxy]-3,5-diiodophenyl]- (1951-25-3) |
Safety
| Symbol(GHS) |

|
| Signal word | Warning |
| Hazard statements | H302 |
| Precautionary statements | P264-P270-P301+P312-P330-P501 |
| Hazard Codes | Xn |
| Risk Statements | 20/21/22 |
| Safety Statements | 36 |
| WGK Germany | 3 |
| RTECS | OB1361000 |