Side effects of Amodiaquine
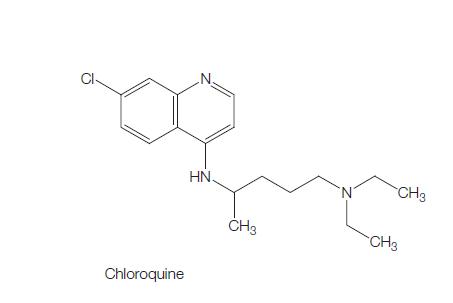
Amodiaquine is a 4-aminoquinoline which has been used widely since the early 1950s to treat and prevent Plasmodium falciparum malaria. Although a 7-chloro-4-amino congener of chloroquine, it often remains effective against chloroquine-resistant parasites. It was also effective against P. vivax and other non-falciparum malaria species. Historically, amodiaquine has largely been used in Africa as monotherapy for treatment of malaria. Amodiaquine is more palatable than chloroquine, and has therefore had a treatment role in children.

Uses
Amodiaquine was more widely used for malaria prophylaxis until fatalities from hepatotoxicity and agranulocytosis led to its removal from the WHO Essential Drug List in 1990. Subsequent reviews, however, suggested that the risk associated with malaria treatment was minimal, and emerging chloroquine resistance led to an increasing treatment role for amodiaquine. More recently, worldwide amodiaquine use has increased again as a partner drug in combination with artemisinins.
Mechanism of action
Amodiaquine is thought to have a similar mechanism of action to chloroquine, both acting as blood-stage schizonticides. During intraerythrocytic growth and replication of malaria, hemoglobin is utilized as the principal source of nutrition, and its digestion takes place within the parasitic digestive vacuole. The digestion of hemoglobin leads to the formation of heme, which is immediately oxidized to ferriprotoporphyrin IX (FPIX). FPIX is highly toxic to cells and leads to increased membrane permeability and cell lysis. The detoxification of FPIX is therefore crucial to parasite survival, and is achieved through the conversion of FPIX to the inactive and insoluble crystalline hemozoin (malaria pigment). Although the antimalarial activity of amodiaquine is incompletely understood, it is believed that, like chloroquine, amodiaquine accumulates within the digestive vacuole, and binds with high affinity to FPIX to prevent its detoxification to hemozoin.
Inhibition of plasmepsin, a protease involved in the digestion of heme within the digestive vacuole, has been shown to be inhibitory to the action of chloroquine, suggesting that unless the FPIX is formed by the oxidation of heme, the chloroquine will not be able to act by inhibiting FPIX breakdown. This has been repeated in studies of many quinoline antimalarials, including amodiaquine.
Bioavailability
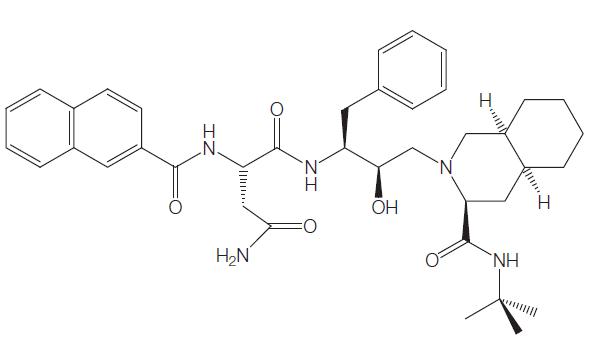
Amodiaquine is rapidly absorbed after oral administration with a mean time to peak plasma concentration of 30 minutes. Amodiaquine undergoes extensive first-pass hepatic metabolism, and is rapidly converted in the liver to its active metabolite DEAQ, predominantly by the action of CYP2C8 enzyme. Amodiaquine is extensively protein bound.
Amodiaquine (as distinct from chloroquine) is rapidly cleared from the blood with a half-life of 5 hours. Indeed, no amodiaquine can routinely be detected in the plasma 12 hours after dosing. There are different estimates of the terminal elimination halflife of DEAQ, between 9 and 18 days and 1–3 weeks. In a pediatric population, it was found to be shorter at 3–12 days. The DEAQ elimination half-life is shorter than for chloroquine.Amodiaquine absorption is not influenced by food – an advantage when compared with another ACT partner drug, lumefantrine, as this should be taken with fatty food.
Side effects
Chloroquine and amodiaquine generally share similar toxicities, albeit with some significant differences. Overall, the most frequent adverse amodiaquine events are nausea, vomiting and pruritus. Other reviews of amodiaquine and chloroquine, used alone and in combination with SP, reported no significant differences in adverse events. Less abdominal pain and pruritus may occur with amodiaquine than chloroquine.
Cardiac and neurologic effects
Amodiaquine causes cardiac conduction disturbances that are not regarded as clinically significant. Bradycardia occurs around the second day of treatment and correlates with the time of peak cumulative plasma concentration. Unlike chloroquine, there have been no reports of cardiovascular symptoms following overdose of amodiaquine. Large doses of amodiaquine have, instead, been reported to cause syncope, spasticity, convulsions, and involuntary movements.