Hydroxychloroquine: mechanisms of action, pharmacokinetics and safety
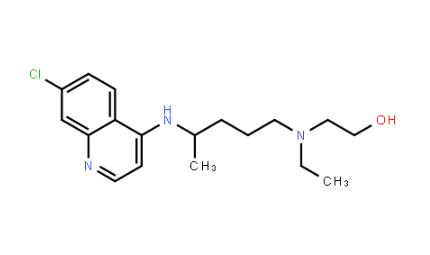
General Description
Hydroxychloroquine has multiple mechanisms of action in the treatment of systemic lupus erythematosus (SLE) and antiphospholipid syndrome. It interferes with immune response by inhibiting TLR7 and TLR9 receptors, disrupting T cell activation, and inhibiting proinflammatory cytokines. Hydroxychloroquine also inhibits lysosome-dependent autophagy and prevents thrombosis in antiphospholipid syndrome. In terms of pharmacokinetics, Hydroxychloroquine is well-absorbed, metabolized in the liver, and eliminated through the kidneys. It has a long elimination half-life and accumulates in tissues. Adverse effects include ocular complications, cardiovascular side effects, and cutaneous complications. Regular monitoring and caution are necessary to minimize these risks. Overall, understanding the diverse mechanisms and pharmacokinetics of Hydroxychloroquine is crucial for its safe and effective use in the treatment of autoimmune diseases.

Figure 1. Tablets of hydroxychloroquine
Mechanisms of action
Hydroxychloroquine has various mechanisms of action in the treatment of systemic lupus erythematosus (SLE) and antiphospholipid syndrome. In SLE, Hydroxychloroquine interferes with the immune response at different levels. It inhibits the signaling of TLR7 and TLR9 receptors, which are involved in the activation of innate immunity. Hydroxychloroquine either inhibits endosomal acidification or directly binds to nucleic acids, preventing their binding to TLRs. Hydroxychloroquine also accumulates in lysosomes of antigen-presenting cells, inhibiting the presentation of peptides to T cells. Additionally, it inhibits proinflammatory cytokines and disrupts T cell receptor-dependent calcium signaling, leading to the suppression of T cell activation. Hydroxychloroquine is also a potent inhibitor of lysosome-dependent autophagy, impairing protein degradation crucial for activating innate and acquired immunity. In antiphospholipid syndrome, Hydroxychloroquine reduces the risk of thrombosis by inhibiting the binding of antiphospholipid antibody complexes to phospholipid bilayers. It can restore the binding of annexin A5, an anticoagulant protein disrupted by antiphospholipid antibodies, thus protecting its activity. These mechanisms highlight the diverse immunomodulatory and antithrombotic properties of Hydroxychloroquine, which have implications for the treatment of autoimmune diseases and antiphospholipid syndrome. 1
Pharmacokinetics
Hydroxychloroquine is a weak base that is well-absorbed from the gastrointestinal tract. It has a good bioavailability and is metabolized in the liver by cytochrome P450 enzymes to several metabolites. Hydroxychloroquine is mainly eliminated through the kidneys, with a long elimination half-life of approximately 40-60 days. The drug is extensively distributed and sequestered in tissues, leading to slow accumulation and delayed steady-state concentrations. Inter-individual pharmacokinetic variability can result in variable drug concentrations after standard doses. Potential drug interactions have been identified with D-penicillamine and cimetidine, but not with aspirin, ranitidine, or imipramine. Drugs that induce or inhibit cytochrome P450 enzymes may affect Hydroxychloroquine blood levels. Hydroxychloroquine has metabolic effects, improving beta cell function and insulin sensitivity. This may explain its association with a lower risk of type 2 diabetes. However, caution is advised in patients taking insulin to prevent severe hypoglycemia. In the treatment of systemic lupus erythematosus (SLE), the initial dosage of Hydroxychloroquine is usually 400 mg orally once or twice a day, with therapeutic effects appearing after weeks or months. The maintenance dose ranges from 200 to 400 mg per day. There is debate about the optimal dosing strategy, with some suggesting dosing based on actual body weight and others favoring ideal body weight. Overall, understanding the pharmacokinetics of Hydroxychloroquine is important for achieving therapeutic efficacy and minimizing adverse effects in patients with SLE. 2
Safety
Hydroxychloroquine is generally considered to be a safe drug, but like any medication, it can cause adverse events. The side effects of Hydroxychloroquine are often dose-dependent, and many adverse events result from intentional or unintentional over-dosage. Patients with specific conditions such as allergy, psoriasis, porphyria, and alcoholism are more susceptible to cutaneous side effects. Children are particularly vulnerable to side effects even with small over-dosages of chloroquine. The most serious side effects of Hydroxychloroquine include ocular complications, such as corneal deposits and retinopathy, which can lead to visual disturbances and vision loss. The risk of retinal toxicity increases with high doses and long durations of use, particularly with cumulative doses higher than 1000 g of Hydroxychloroquine. Cardiovascular side effects, though rare, can manifest as cardiomyopathy or conduction system abnormalities, and risk factors for Hydroxychloroquine-induced cardiotoxicity include older age, longer duration of therapy, pre-existing cardiac disease, and renal insufficiency. Cutaneous complications may include various dermatologic adverse events and, in exceptional cases, life-threatening epidermal necrolysis. Monitoring for these potential side effects is crucial, and patients and prescribing physicians should be informed about the risks of toxicity. Regular annual screening, including visual field tests, optical coherence tomography, and electroretinogram, is recommended for early detection of retinopathy. Additionally, caution should be exercised in patients with risk factors for cardiotoxicity. 3
Reference
1. Ponticelli C, Moroni G. Hydroxychloroquine in systemic lupus erythematosus (SLE). Expert Opin Drug Saf. 2017 Mar;16(3):411-419.
2. Rainsford KD, Parke AL, Clifford-Rashotte M, et al Therapy and pharmacological properties of hydroxychloroquine and chloroquine in treatment of systemic lupus erythematosus, rheumatoid arthritis and related diseases. Inflammopharmacology. 2015;23 (5):231–269.
3. Smith ER, Klein-Schwartz W. Are 1-2 dangerous? chloroquine and hydroxychloroquine exposure in toddlers. J Emerg Med. 2005;28 (4):437–443.
Related articles And Qustion
Lastest Price from Hydroxychloroquine manufacturers

US $10.00/KG2025-04-21
- CAS:
- 118-42-3
- Min. Order:
- 100KG
- Purity:
- 99%
- Supply Ability:
- 100 mt
US $150.00/kg2025-04-21
- CAS:
- 118-42-3
- Min. Order:
- 1kg
- Purity:
- 99%
- Supply Ability:
- 500kg