Cyclophosphamide in Dermatology: Dosage, Pharmacokinetics and Clinical Application
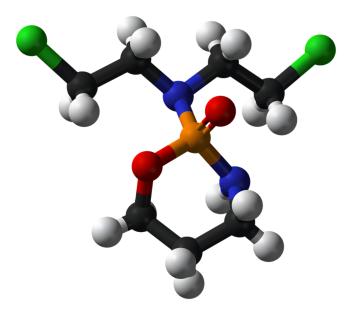
General Description
Cyclophosphamide is commonly used in dermatology as a steroid-sparing adjunct for severe autoimmune skin diseases. It can be administered orally or intravenously, along with prednisolone, to induce remission. Oral doses range from 1 to 5 mg/kg per day, while IV pulse therapy involves doses of 500 mg or 10-15 mg/kg at 3-4 week intervals. Cyclophosphamide is well-absorbed when taken orally and metabolized in the liver, with renal excretion. It is effective for treating severe manifestations of autoimmune diseases, although high-quality evidence in dermatology is limited. Healthcare professionals need to carefully evaluate risks and monitor for adverse effects.
Figure 1. Injection of cyclophosphamide
Dosage in Dermatology
As a steroid-sparing adjunct for the treatment of autoimmune skin diseases, cyclophosphamide is administered either orally or intravenously, usually alongside oral prednisolone, with the aim of inducing remission. Oral cyclophosphamide doses range from 1 to 5 mg/kg per day, and rarely exceed 2-2.5 mg/kg per day, while the duration of therapy can vary. Hospitalization is not required for oral administration, it is cheaper than i.v. administration, and dose-adjustments can be made for dose-limiting side-effects. I.v. cyclophosphamide pulse therapy (CPT) typically involves doses of 500 mg or 10-15 mg/kg of cyclophosphamide, administered at 3-4 weekly intervals. Some authors recommend increasing the dose until the third infusion, after which the dose is maintained. The frequency of pulses is often tapered to the patient's response, and the duration of treatment is variable. Dexamethasone-cyclophosphamide combined pulse therapy (DCP) is used for the treatment of pemphigus, involving the administration of 100 mg of dexamethasone daily for 3 consecutive days, and 500 mg-1 g or 10-15 mg/kg of cyclophosphamide on one of these days. Similarly, methylprednisolone with cyclophosphamide has also been used for refractory pemphigus. Cyclophosphamide is often part of combined regimens for cutaneous T-cell lymphomas. 1
Pharmacokinetics
Cyclophosphamide is a medication that is used in the treatment of autoimmune diseases and primary cutaneous T-cell lymphomas. It is available both orally and intravenously, and is well-absorbed when taken orally, with peak concentration attained within 1-3 hours. Cyclophosphamide is metabolized in the liver by cytochrome P-450 enzymes to form its active metabolites, which exert DNA-alkylating effects. These active metabolites are detoxified by aldehyde dehydrogenase (ALDH) enzymes, particularly ALDH1, as well as glutathione-S-transferase. Cyclophosphamide and its metabolites are renally excreted. Individual variability in CYP and ALDH1 expression, younger age, and hepatic dysfunction may alter cyclophosphamide metabolism, but there is no evidence that the dose of cyclophosphamide needs to be reduced in the context of hepatic dysfunction. Renal impairment may increase systemic drug exposure, but available data does not demonstrate clinically relevant changes. Before administering the drug, the severity of renal impairment should be considered. There are some drug-drug interactions with cyclophosphamide, which are listed in Table 2. Overall, understanding the pharmacokinetics of cyclophosphamide is important for healthcare professionals in order to ensure safe and effective use of this medication in the treatment of severe autoimmune diseases and primary cutaneous T-cell lymphomas. 2
Clinical Applications
Cyclophosphamide is a medication that finds its clinical applications in dermatology primarily as a steroid-sparing adjunct for severe or refractory autoimmune diseases. This is especially relevant when other immunosuppressive medications like azathioprine (AZA) or mycophenolate mofetil (MMF) have failed or are contraindicated. Additionally, cyclophosphamide is used in chemotherapeutic regimens for primary cutaneous T-cell lymphomas. The effectiveness of cyclophosphamide in treating severe manifestations of autoimmune diseases such as lupus, vasculitides, and systemic sclerosis has been well-established in the rheumatological literature. However, there is a relative scarcity of high-quality evidence supporting its therapeutic application specifically in dermatology. Despite the limited evidence, cyclophosphamide is still considered an important treatment option in dermatology for patients with severe autoimmune diseases that do not respond to other conventional therapies. It is crucial for healthcare professionals to carefully evaluate the risks and benefits of using cyclophosphamide and closely monitor patients for potential adverse effects, as this medication can have significant side effects, including bone marrow suppression and increased susceptibility to infections. 3
Reference
1. Bressan AL, da Silva RS, Fontenelle E et al Immunosuppressive agents in dermatology. An Bras Dermatol. 2010; 85: 9-22.
2. De Jonge ME, Huitena AD, Rodenhuis S et al Clinical pharmacokinetics of cyclophosphamide. Clin. Pharmacokinet. 2005; 44: 1135-1164.
3. Kim J, Chan JJ. Cyclophosphamide in dermatology. Australas J Dermatol. 2017; 58(1): 5-17.
You may like
Related articles And Qustion
See also
Lastest Price from Cyclophosphamide manufacturers

US $0.00/kg2025-09-30
- CAS:
- 50-18-0
- Min. Order:
- 1kg
- Purity:
- 98%
- Supply Ability:
- 1000kg

US $0.00-0.00/kg2025-04-21
- CAS:
- 50-18-0
- Min. Order:
- 1kg
- Purity:
- 98%min
- Supply Ability:
- 1000kg