Aviptadil(VIP) is a neuropeptide consisting of 28 aa residues, with
wide distribution in the central and peripheral nervous systems. VIP has a broad spectrum of biologic actions, and acts
as a neurotransmitter or neuromodulator and also as a
hormone. VIP was first discovered as a smooth muscle-relaxant
vasodilator peptide in the lung; it was isolated from the
porcine intestine in 1970. Its original label as a
“candidate gastrointestinal hormone” was soon replaced
by its new and apparently true identity as a neuropeptide
with neurotransmitter and neuromodulator properties.
VIP possesses two segments of secondary structures: a
random coil structure in the N-terminal region between
positions 1 and 9, and a long α-helical structure in the
C-terminal region stretching from position 10 to its
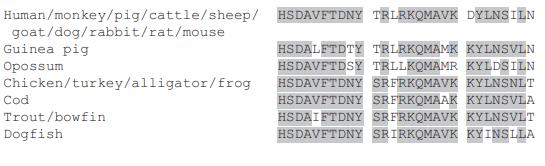
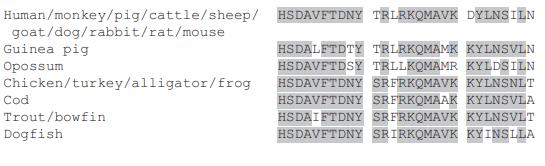
C-terminus. The primary structure of VIP is highly conserved in
vertebrates with complete identity among mammals
except for the guinea pig and opossum. Mr 3326, pI >11. VIP is soluble in water to 20mg/mL.
Gene, mRNA, and precursor
The human VIP gene, VIP, location 6q25.2, contains
seven exons. Each exon encodes a distinct functional
domain of the VIP precursor. The VIP precursor polypeptide (preproVIP) contains several additional biologically active peptides, including peptide histidine
isoleucine (PHI, found in nonhuman mammals), peptide
histidine methionine (PHM, the human equivalent of
PHI), and peptide histidine valine (PHV, a C-terminally
extended form of PHI and PHM).
VIP and PACAP share a wide spectrum of biological
activity as well as common receptors belonging to the
class II of GPCR. Three VIP or PACAP receptor types,
which are derived from different genes, are recognized,
namely VPAC1, VPAC2, and PAC1. Two of these receptors, VPAC1 and VPAC2, share a high binding affinity in
the nanomolar range for VIP and PACAP. A third receptor type, PAC1, has been characterized for its high affinity
for PACAP, but low affinity for VIP.
Aviptadil gene expression is stimulated by dibutyryl cAMP
and by increased PKC activity induced by tumorpromoting phorbol esters. When acting together, cAMP
and phorbol esters synergistically stimulate VIP gene
transcription via different sites on the gene.
Signal transduction pathway
By binding to VIP, VPAC acts on the Gs protein and
activates PKA via elevation of AC activity and production of cAMP (cAMP-dependent pathway). PKA either
inhibits phosphorylation of the downstream MAP/ERK
kinase or promotes phosphorylation of cAMP response
element binding protein (CREB), which finally leads to
the inhibition of NF-κB. Meanwhile, studies have also
identified a pathway that inhibits the nuclear entry of
NF-κB through VPAC signaling, which inhibits IκB phosphorylation (cAMP-independent pathway).
VIP is extensively distributed in central and peripheral
tissues, where it acts as a neurotransmitter and neuromo�dulator.8 The main activity of VIP is vasodilatation. VIP
induces the dilation of vessels, which results in increased
blood flow, decreased peripheral vascular resistance, and
hypotension. While VIP has a suppressive effect on the
intestinal smooth muscle, it exerts relaxant effects on
the lower esophageal sphincter, the sphincter of Oddi,
the anal sphincter, and the bronchial smooth muscle. In
the small intestine, VIP facilitates the secretion of electrolytes and aqueous liquid. In the stomach, it inhibits gastric secretion. In the pancreas, VIP facilitates the external
secretion of bicarbonic acid and aqueous liquid from pancreatic epithelial cells, and facilitates enzyme secretion
from acinar cells. VIP promotes the secretion of both insulin and glucagon in a glucose-dependent manner. VIP is
broadly distributed in the central nervous system, especially in the hypothalamus and pituitary anterior lobe,
and is associated with the regulation of pituitary hormones. VIP is produced by lymphoid tissue and exerts
a wide spectrum of immunological functions, controlling
the homeostasis of the immune system through different
receptors expressed in various immunocompetent cells. VIP acts as a growth factor. It functions as a proliferative
factor in normal tissue cells as well as in cancer cells. VIP
might inhibit apoptosis by stimulating the expression of
the apoptosis-inhibiting gene Bcl2 or by inhibiting the
activity of caspase 3.
Various diseases have been reported to involve VIP
activity, including bronchial asthma, transmission of
pain, cluster headaches, Alzheimer’s disease, Parkinson’s
disease, and brain injury.
Pulmonary hypertension;Erectile dysfunction
Vasoactive Intestinal Peptide human, porcine, rat has been used as an immunogen to analyze the immunohistochemical reactions. It has also been used in cell migration assay.
Vasoactive intestinal peptide (VIP) is widely distributed inthe body and is believed to occur throughout the gastrointestinaltract. It is a 28-residue polypeptide with structuralsimilarities to secretin and glucagon. It causes vasodilatationand increases cardiac contractibility. VIP stimulates bicarbonatesecretion, relaxes gastrointestinal and othersmooth muscles, stimulates glycogenesis, inhibits gastricacid secretion, and stimulates insulin secretion. Its hormonaland neurotransmitter role has been investigated.
VIP (Vasoactive intestinal peptide) possesses anti-inflammatory and immunomodulatory functions. It controls the pathogenesis of rheumatoid arthritis. It is also involved in neuroblastoma differentiation, and pancreatic insulin secretion. Vip exhibits its function through G-protein coupled receptors. Some of the other important actions of VIP is associated with the digestive, respiratory, cardiovascular and reproductive systems.
28-peptide that is structurally related to
secretin and glucagon. It has a diverse
biological actions. It has orphan drug
status for the treatment of acute
esophageal food impaction.
Several clinical trials have been reported regarding the
use of VIP or its analog for asthma and sarcoidosis. In an
open clinical Phase II study, patients with histologically
proven sarcoidosis and active disease were treated with
nebulized VIP. VIP inhalation was safe and well tolerated, and significantly reduced the production of tumor
necrosis factor-α by cells isolated from the bronchoalveolar lavage fluids of these patients.
Vasoactive Intestinal Peptide Synthetic is a single, non-glycosylated polypeptide chain containing 28 amino acids, having a molecular mass of 3325 Dalton and a Molecular formula of C147H238N44O42S .