Pharmacology and mechanism of action
Dehydroemetine, is a derivative of emetine and has similar pharmacological properties, but it is considered to be less toxic. Dehydroemetine acts against Entamoeba histolytica in tissue and has little effect on amoeba confined to the lumen of the bowel. It has a direct amoebicidal effect in vitro by interfering with the mRNA translocation along the ribosome, which causes inhibition of protein synthesis
[1].
Indications
Serious intestinal amoebiasis and amoebic hepatitis with liver abscess. Dehydroemetine is usually given with chloroquine. It is only indicated when other safer drugs are not available or contraindicated.
Side effects
Side effects are similar to those caused by emetine, but they are milder and less frequent. They are largely gastrointestinal, cardiac and neuromuscular reactions. Gastrointestinal reactions include nausea, vomiting, and abdominal pain. Neuromuscular effects are generalized muscle weakness, muscle pain and stiffness of the limbs and neck. Cardiac effects include fall in blood pressure, tachycardia and ECG changes of T-wave flattening or inversion
[2,3]. The injection of dehydroemetine is painful and the formation of an abscess is common
[2].
Contraindications and precautions
Patients with heart, muscle, or neurological diseases or in poor general condition should be treated with great caution. Dehydroemetine should always be given under medical supervision. Strenuous exercise should be forbidden until 4–5 weeks after completion of therapy
[4]. Dehydroemetine should not be given earlier than 1.5–2 months after emetine treatment because of cardiotoxicity.
Previous recommendations to use a contact amoebicide (e.g. di-iodohydroxyquinoline) together with an oral drug preparation can no longer be supported. The hydroxyquinolines have been withdrawn from most markets because of their potential risk of inducing subacute myelo-optic neuropathy (SMON).
Interactions
There have been no reports.
Preparations
Available as dehydroemetine hydrochloride: 100 mg salt equals 87 mg base.
• Dehydroemetine® (Roche) Ampoules 30 mg/ml, ampoules 60 mg/2 ml.
References
1. Westwood JT, Wagenaar EB (1983). Chinese hamster cells can be reversibly blocked before mitosis with the protein synthesis inhibitor Emetine. J Cell Sci, 59, 257–268.
2. Salem HH, Abd-Rabbo H (1964). Clinical trials with dehydroemetine dihydrochloride in the treatment of acute amoebiasis. J Trop Med Hyg, 67, 137–141.
3. Powell SW, Wilmot AJ, McLeod IN et al. (1965). Dehydroemetine in the treatment of amoebic liver abcess. Ann Trop Med Parasitol, 59, 208–209.
4. Wilmot AJ (1962). Clinical Amoebiasis (Oxford: Blackwell Scientific Publications).
Definition
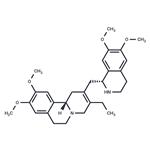
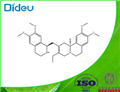
ChEBI: Dehydroemetine is a pyridoisoquinoline which was developed in response to the cardiovascular toxicity associated with emetine and results from the dehydrogenation of the heterotricylic ring of emetine. It is an antiprotozoal agent and displays antimalarial, antiamoebic, and antileishmanial properties. It has a role as an antiprotozoal drug, an antimalarial and an antileishmanial agent. It is a member of isoquinolines, an aromatic ether and a pyridoisoquinoline. It derives from a hydride of an emetan.
Pharmaceutical Applications
The synthetic racemic derivative of the plant alkaloid
emetine. Formulated as the hydrochloride for intramuscular
administration.
Like the parent compound, emetine, it
inhibits
E. histolytica at concentrations of 1–10 mg/L in vitro,
but it is more active than the parent in animal models. Drugresistance
in E. histolytica is rare.
No human pharmacokinetic data are available. A halflife
of 2 days, compared with 5 days for emetine, has been
reported. There is selective tissue binding and accumulation
in the liver, lung, spleen and kidney.
It is considerably less toxic than emetine, possibly because
it is more rapidly eliminated. Nevertheless, nausea, vomiting,
diarrhea and abdominal cramps frequently occur.
Neuromuscular effects have also been reported. More serious
cardiotoxic effects can lead to electrocardiogram (EGG)
changes, tachycardia and a drop in blood pressure.
It was formerly used as a second-line treatment in severe
intestinal or hepatic amebiasis, but is no longer recommended
for use.