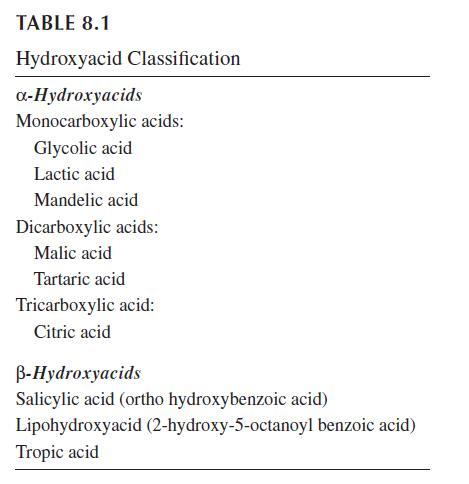
Uses in Cosmetics of Hydroxyacids
Hydroxyacids are well known for their use in the cosmetics industry. They are often found in products that aid in the reduction of wrinkles, that soften strong, defining lines, and that improve the overall look and feel of the skin. They are also used as chemical peels. AHAs have effective results through continuous treatment in the cosmeceutical industry.
Effects on Corneocyte Cohesion and Stratum Corneum Functions
During the formation and maturation of the stratum corneum (SC), the intercellular binding by desmosomes
becomes modified into corneodesmosomes. Their numbers usually decrease towards the surface
of the skin, most notably during the stratum compactum to stratum disjunctum transition. In xerotic,
scaly, and ichthyotic conditions, ordered desquamation is impaired because desmosomes persist up to
the outer SC leading to the unruly accumulation of corneocytes and to skin scaling and flacking. Environmental conditions often influence these skin conditions.
Salicylic acid is the time-honored BHA used in dermatology to improve xerotic and scaly conditions.
Although this compound at low and medium concentrations exhibit little or no effect on the
normal SC, there is evidence that complete corneodesmosome degradation is helped in various xerotic
and ichthyotic disorders. It therefore appears that the term keratolytic applied to such a compound is
a misnomer, while a desmolytic agent would be more appropriate and explicit. The clinical effects of
hydroxyacids on such hyperkeratotic conditions is conveniently assessed using a series of biometrological
methods.
A lipophilic derivative of salicylic acid was designed some years ago. It corresponds to the 2-hydroxy 5-octanoyl benzoic acid, also named lipohydroxyacid (LHA). One of the main targets is clearly the corneodesmosomes which appear to be weakened following altered chemical bonds in the junctional complexes.11–13 Subtle differences in desmolytic activity of salicylic acid and LHA were ascribed to the respective hydrophilic and lipophilic natures of these compounds. LHA is likely to have a potential clinical advantage, as it appears to only interact with the more superficial layers of the SC. In addition, its activity is more closely targeted than that of salicylic acid, because it is channeled into the junction between the corneodesmosome and the corneocyte envelope. By contrast, salicylic acid degrades corneodesmosomes rather indiscriminately.
Various AHAs, particularly lactic acid and glycolic acid in the medium range of concentrations, have
profound inhibitory effects on corneocyte cohesion. The usefulness of such formulations in xerotic
and allied conditions is beyond doubt.The precise mechanisms of AHA action are poorly documented.
A desirable pH for inducing desquamation with AHA application apparently lies between 2.8 and 4.8.
The pH changes at the skin surface persist several hours following applications and affect a number of
SC layers according to the AHA concentration. A discrete superficial lytic effect in corneodesmosomes occurs in response to low dosages. In other circumstances, when an appropriate amount of a given AHA
is topically applied, the SC abruptly becomes detached at its lowermost levels within a couple of days,
and desquamation occurs as large flakes or sheets. In such instances, no disaggregation of corneocytes
is apparent at the upper SC levels. These changes result in skin peeling.16 To explain this event, speculation
has been made on the interaction between AHAs and various enzymatic processes involved in the
maturation and disaggregation of the SC.
In addition to the therapeutic effect of the various hydroxyacids improving hyperkeratotic disorders,
the same products yield cosmetic benefits by increasing plasticization and flexibility of the SC without
impairing the barrier function.This barrier function was even reported to be improved by some
AHAs, leading to increased resistance to SLS-induced skin irritation. The latter beneficial effect was
not equal for all hydroxyacids, being more marked for AHAs characterized by antioxidant properties.
A similar protection was not provided by applications of salicylic acid.
Peeling and Caustic Effects
When applied to the skin at high concentrations, AHAs may cause necrosis and detachment of keratinocytes corresponding to exogenous epidermolysis. Such an injury results in a chemical peel depending primarily on the disruption of the skin pH. The farther away from the physiological pH, the greater the caustic effect, the greater the risk of adverse events, but the more likely the patient receives the resurfacing benefits of the peeling agents. A tolerable sense of burning and itching is often experienced by the patients.
The indications of such treatment modality encompass the destruction of slightly elevated seborrheic and actinic keratoses. The full-strength preparation must be applied carefully and exactly to the target lesions in an office procedure. After a few minutes, the entire lesion is curetted off. Viral warts are similarly eradicated by hydroxyacids in a home-administered treatment, with applications made daily for several days. To shorten the treatment period, the outer portion of the hyperkeratosis should be removed with a scalpel in an office setting.
Hypopigmenting Effect
Glycolic acid peels are a useful adjunctive treatment of epidermal hypermelanosis such as in melasma and acne scars. The association of 10% glycolic acid and 2% hydroquinone improves this disorder. Still another therapy combines 5% glycolic acid and 2% kojic acid. It is thought that AHAs act like penetration enhancers and accelerate the epidermal turnover.
Acne and Pseudofolliculitis Treatment
Salicylic acid is listed among active products to treat acne.26 However, clearcut evidence for a significant benefit at low concentration in well-controlled experimental and clinical trials is scant. Similarly, medium concentrations of AHAs such as glycolic acid, lactic acid, and mandelic acid are employed twice daily to improve mild acne. It has been postulated that hydroxyacids promote dislodgement of comedones and prevent their formation as well. Many of these treatments await validation by independent controlled studies. In our experience, the lower AHA concentrations as present in some cosmetic products exhibit little or no effect whatsoever on acne and comedones.
Another modality of acne treatment consists of using high concentrations of glycolic acid in an office setting. The procedure has to be repeated weekly or so. In addition to the comedolytic effect, the higher hydroxyacid concentrations help to unroof pustules and affect the follicular epithelium. The skin condition improvement is reported to be precipitous while patients were taking oral tetracyclines. Discomfort, mild diffuse erythema, and fine scaling are often experienced by patients. In addition, there is a risk for stronger irritation leading to a papular and perifollicular erythema that commonly persists for a few weeks.
A 2% LHA formulation was shown to exert a comedolytic effect in acne-prone subjects. The lipophilic properties of LHA allow maximum concentration inside the SC, particularly in the sebumenriched infundibulum of the pilosebaceous units. Thus, the compound is likely to be trapped in lesional sebaceous follicles which represent a critical therapeutic target in comedonal acne. The product has shown efficacy in preventing post-summer comedonal acne and in treating mild acne. LHA has the capacity to decrease both the number and the size of the cornified follicular plugs induced by intense ultraviolet (UV) light exposure.The combination of the LHA formulation with a retinoic acid cream every other evening results in the overall decrease in the functional and physical intolerance reactions.29 Pseudofolliculitis is another related disorder that can be improved by topical AHA treatment. Rosacea might similarly benefit from the combination of an evening AHA cream and a sun-protective daytime preparation.
Boosting Skin Physiology
One fascinating aspect in the effects of hydroxyacids is the boosted physiology that was claimed to occur in the epidermis and dermis.31,32 Accordingly, some of these compounds are used to correct skin atrophy and to induce a gradual reduction in the aging signs including pigmentary changes33 and wrinkles of fine and moderate depths.32,34–36 However, only a few controlled clinical trials and experimental studies have been conducted to validate these observations.
After a few days of application of 12% glycolic acid at low pH, fine wrinkles of the face may vanish as a result of the irritation and dermal edema. Besides the untoward immediate effect of stinging, such smoothing effect is rapidly alleviated upon arrest of the topical treatment. Furthermore, in long-term applications, there is some concern regarding the occurrence of chronic low-grade inflammation producing reactive oxygen species (ROS) damaging cells as well as collagen and elastic fibers. However, signs of repair and reverse changes of aging and photoaging were reported on long-term therapy. Such findings were not confirmed in other studies, which rather indicated an almost absence of AHA effects on major skin aging features. In fact, deposits of glycosaminoglycans in the dermis result from inflammation which has been mistakenly interpreted as a correction of aging. A comparative controlled study showed that tretinoin was more active than medium concentrations of glycolic acid in the improvement of the facial skin tensile properties. It should be noted that the combination of tretinoin and AHAs may be beneficial in improving the aspect of photoaged skin.
In contrast with salicylic acid, low concentrations of LHA elicit a dermo-epidermal stimulation, leading to increased keratinocyte proliferation and epidermal thickness. Such effects are more evident in older skin and remain within the physiologic range of normal skin. At the difference with other AHAs and BHAs, angiogenesis is moderately increased by LHA. An increased number of Factor XIIIa-positive dermal dendrocytes occurs after topical applications of AHAs and LHA. These cells may influence the metabolism of fibroblasts and endothelial cells. The increase in Factor-XIIIa expression may somehow relate increased vascularity and dermal improvements following LHA and tretinoin treatments in photoaged patients.
Safety
Adverse reactions following LHA applications are mostly represented by stinging sensations without any other clinical and histopathological signs of irritation. However, the higher concentrations are responsible for severe redness, swelling (especially in the area of the eyes), burning, blistering, bleeding, rash, itching, and skin discoloration. Their long-term effects are unknown. It has been claimed that BHAs are effective as exfoliants without the occasional irritation associated with the use of AHAs.
Some AHA users suffer from greater reactivity to sun exposure. Indeed, it was reported that subjects who receive AHA products in the presence of UV radiation experience twice the cell damage in areas where the AHA is applied than controls.
The U.S. FDA stated that AHAs were readily absorbed into the skin at varying rates. The most rapid absorption occurred with AHAs at lower pH. The safety of salicylic acid used as a cosmetic ingredient was evaluated by the U.S. FDA and the Cosmetic Ingredient Review (CIR). They concluded that products containing salicylic acid should contain a sunscreen or bear directions advising consumers to use other sun protection.
Conclusions
AHAs and BHAs enjoy tremendous interest in dermatology and cosmetology. These compounds under the presentation of peels and home regimens are recognized as important preventive means and adjunctive therapy in a variety of skin conditions. Thus, they attract media attention and consumer curiosity. Claims and proven effects are contradictory by some aspects. LHA had appeared effective in the treatment of signs of skin aging and in acne treatment without the occasional irritation associated with the use of AHAs. Much remains to be learned, and speculations must be turned to facts. Improved regimens capitalizing on the various beneficial effects of hydroxyacids should be explored. Synergistic effects can be expected with some other compounds. Considering the safety status, consumers who use AHA and BHA products should follow some precautions about ultraviolet radiation exposure.
REFERENCES
1. Lévêque JL, Corcuff P, Gonnord G et al. Mechanism of action of a lipophilic derivative of salicylic acid
on normal skin. Skin Res Technol 1995;1:115–22.
2. Lévêque JL, Corcuff P, Rougier A, Piérard GE. Mechanism of action of lipophilic acid derivative on
normal skin. Eur J Dermatol 2002;12:S35–8.
3. Corcuff P, Fiat F, Minondo AM, Lévêque JL, Rougier A. A comparative ultrastructural study of hydroxyacids
induced desquamation. Eur J Dermatol 2002;12:S39–43.
4. Yener G, Baitokova A. Development of a w/o/w emulsion for chemical peeling applications containing
glycolic acid. J Cosmet Sci 2006;57:487–94.
5. An S, Lee E, Kim S et al. Comparison and correlation between stinging responses to lactic acid and
bioengineering parameters. Contact Dermatitis 2007;57:158–62.
6. Xhauflaire-Uhoda E, Piérard-Franchimont C, Piérard GE. Effects of various concentrations of glycolic
acid at the corneoxenometry and collaxenometry bioassays. J Cosmet Dermatol 2008;7:194–8.
7. Redaelli A. Cosmetic use of polylactic acid for hand rejuvenation: Report on 27 patients. J Cosmet
Dermatol 2006;5:233–8.
8. Oresajo C, Yatskayer M, Hansenne I. Clinical tolerance and efficacy of capryloyl salicylic acid peel
compared to a glycolic acid peel in subjects with fine lines/wrinkles and hyperpigmented skin. J Cosmet
Dermatol 2008;7:259–62.
9. Thiéry G, Coulet O, Adam S, Guyot L. Poly-L-lactic-acid filling on facial lipoatrophy in HIV+ patients
under tritherapy. Rev Stomatol Chir Maxillofac 2008;109:103–5.
10. Effendy I, Kawangsukstith C, Lee JY, Maibach HI. Functional changes in human stratum corneum
induced by topical glycolic acid: Comparison with all-trans retinoic acid. Acta Dermatol Venereol
1995;75:455–8.