The Pharmacodynamics of L(-)-Epinephrine and Its Role in Anaphylaxis Management
General Description
L(-)-Epinephrine is a sympathomimetic drug that acts on effector cells by mimicking sympathetic nervous system actions. It activates beta-1 receptors, increasing heart rate, myocardial contractility, and renin release. Additionally, it activates beta-2 receptors, leading to bronchodilation, vasodilation, tocolysis, and increased aqueous humor production. Epinephrine is effective in managing asthma exacerbations and reducing croup symptoms. It provides relief from pruritus, urticaria, angioedema, and gastrointestinal/genitourinary symptoms associated with anaphylaxis. Mechanistically, it acts on alpha receptors to minimize vasodilation and increases vascular permeability during anaphylaxis. Epinephrine also acts as a histamine antagonist. Its action on beta-adrenergic receptors induces bronchial smooth muscle relaxation, addressing bronchospasm and dyspnea. Moreover, it increases blood sugar levels and promotes glycogenolysis. L(-)-Epinephrine undergoes rapid metabolism and elimination, primarily through enzymatic transformation and subsequent excretion in urine. The plasma half-life is approximately 2-3 minutes. Intravenous administration produces an immediate response, while subcutaneous or intramuscular administration allows for sustained effects. Overall, L(-)-Epinephrine's pharmacodynamics make it a valuable medication for managing asthma, croup, anaphylaxis, and allergic reactions.

Figure 1. Injection of L(-)-Epinephrine
Pharmacodynamics
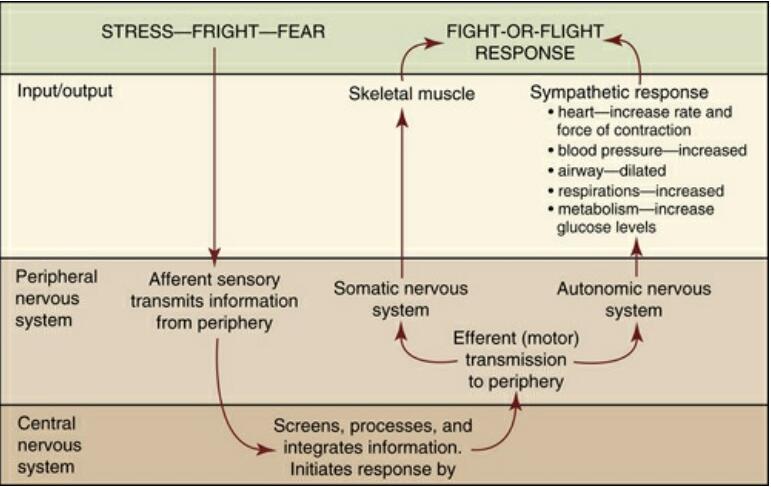
L(-)-Epinephrine, a sympathomimetic drug, acts on effector cells by mimicking sympathetic nervous system actions, except for facial arteries and sweat glands. It activates beta-1 receptors to increase heart rate, myocardial contractility, and renin release. Meanwhile, beta-2 receptors produce bronchodilation, vasodilation, tocolysis, and increased aqueous humor production. Epinephrine is useful in managing asthma exacerbations when used as an adjunct treatment. Moreover, nebulized epinephrine can significantly reduce croup symptoms within 30 minutes post-treatment. In addition, it provides relief from pruritus, urticaria, and angioedema. Epinephrine can also alleviate gastrointestinal and genitourinary symptoms associated with anaphylaxis because of its relaxing effects on the smooth muscle of the stomach, intestine, uterus, and urinary bladder. Overall, L(-)-Epinephrine has various pharmacodynamic effects that make it a useful drug for managing several medical conditions such as asthma, croup, and anaphylaxis. 1
Mechanism of action
L(-)-Epinephrine exerts its effects by acting on both alpha and beta-adrenergic receptors. It is the most potent activator of alpha receptors, which allows it to minimize vasodilation and increased vascular permeability during anaphylaxis, preventing intravascular fluid loss and hypotension. Furthermore, epinephrine acts as a histamine antagonist, providing relief from allergic reaction symptoms. Additionally, it induces bronchial smooth muscle relaxation through its action on beta-adrenergic receptors, alleviating bronchospasm, wheezing, and dyspnea associated with anaphylaxis. Epinephrine also increases blood sugar levels and promotes glycogenolysis in the liver. These mechanisms of action make L(-)-Epinephrine an essential medication for managing anaphylaxis and allergic reactions, as it addresses multiple aspects of the physiological response to these conditions, including vascular tone, smooth muscle relaxation, and glycemic control. 1,2
Pharmacokinetics
L(-)-Epinephrine undergoes rapid metabolism and elimination in the body. After intravenous (IV) injection, it quickly disappears from the bloodstream. When administered subcutaneously or intramuscularly, it has a rapid onset of action and short duration. Subcutaneous administration during asthmatic attacks can lead to bronchodilation within 5 to 10 minutes, with maximal effects occurring within 20 minutes. Epinephrine is rapidly inactivated primarily through enzymatic transformation to metanephrine or normetanephrine, which are then conjugated and excreted in the urine as sulfates and glucuronides. This metabolic process generates 3-methoxy-4-hydroxy-mandelic acid (vanillylmandelic acid, VMA), which can be detected in the urine. The enzymes catechol-O-methyltransferase (COMT) and monoamine oxidase (MAO) play a significant role in epinephrine's inactivation, with the liver being a primary site for degradation. The majority of the dose is excreted in the urine, with about 40% appearing as metanephrine, 40% as VMA, and smaller amounts as other metabolites. Only a small portion of the drug is excreted unchanged. The plasma half-life of epinephrine is approximately 2-3 minutes, but absorption delays caused by local vasoconstriction from subcutaneous or intramuscular injection may prolong its effects. Intravenous injection produces an immediate and intensified response, while subcutaneous or intramuscular administration allows for sustained effects. 3
Reference
1. Epinephrine FDA label: EPINEPHRINE - epinephrine injection.
2. Pfizer Monograph: EPINEPHRINE INJECTION USP. 2018, Control No.: 213923.
3. EpiPen Adrenaline (Epinephrine) 0.3 mg Auto-Injector. Mylan, ATC code: C01CA24.
Related articles And Qustion
Lastest Price from L(-)-Epinephrine manufacturers

US $1905.00/KG2025-03-26
- CAS:
- 51-43-4
- Min. Order:
- 1KG
- Purity:
- 99%
- Supply Ability:
- 10000kg

US $0.00/kg2025-03-07
- CAS:
- 51-43-4
- Min. Order:
- 1kg
- Purity:
- 0.99
- Supply Ability:
- 20tons