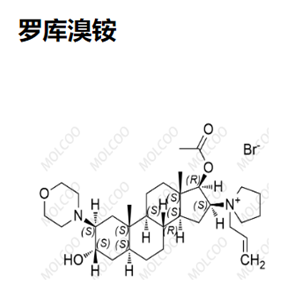
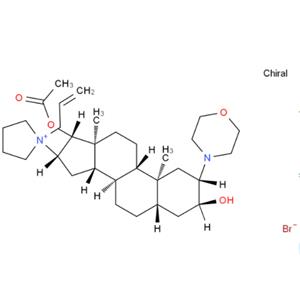
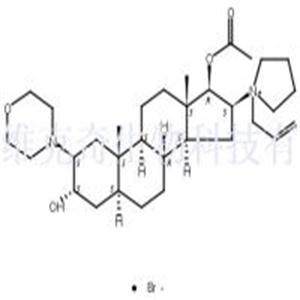
Product Name: Rocuronium Bromide
Synonym: ROCURONIUM BROMIDE;1-[(2b,3a,5a,16b,17b)-17-(Acetyloxy)-3-hydroxy-2-(4-morpholinyl)androstan-16-yl]-1-(2-propenyl)pyrrolidinium Bromide;Esmeron;Org-9426;Zemuron;[3-hydroxy-10,13-dimethyl-2-morpholin-4-yl-16-(1-prop-2-enyl-2,3,4,5-tetrahydropyrrol-1-yl)-2,3,4,5,6,7,8,9,11,12,14,15,16,17-tetradecahydro-1h-cyclopenta[a]phenanthren-17-yl] acetate bromide;ROCURONIUN BROMIDE;Rocuronium Bromide/1-[17B-(acetyloxy)-3a-hydroxy2B-(4-morpholinyl)-5a-androstan-16B-yl]-1-(2-propenyl)pyrrolidinium bromide
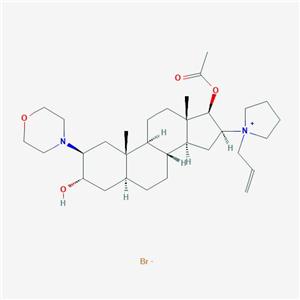
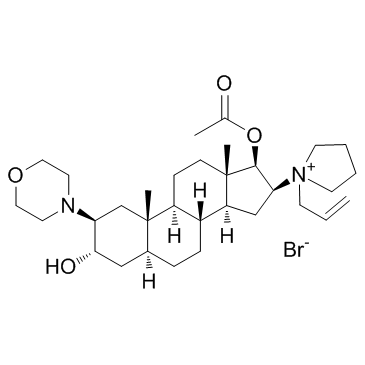
MF: C32H53BrN2O4
MW: 609.68
Product Category: 1;Heterocycles;Steroids;Steroid and Hormone;Acetylcholine receptor;Intermediates & Fine Chemicals;Pharmaceuticals
Melting Point: 162-1640C
Alpha: D20 +18.7° (c = 1.03 in CHCl3)
Storage Temp.: Room temp
Solubility: H2O: soluble100mg/mL, clear, light yellow
Form: neat
Merck: 14,8246
InChlKey: OYTJKRAYGYRUJK-FMCCZJBLSA-M
WGK Germany: 3
Chemical Property: Crystallization; melting temperature of 161~169 °C. [α] D20 + 18.7 ° (C = 1.03, chloroform).
Clinical Evaluation: In anesthetized patients, the strength of producing muscle relaxation effect of Rocuronium bromide is 6-8 times weaker than that of vecuronium and atracurium 6-8 times but with a more rapid onset. This product is usually injected at a dose of 0.5~0.9mg/kg with producing a valid trachea inset effect within 1 minute and having a duration of action similar as vecuronium and atracurium. Compared with succinylcholine, this product has a relatively rapid onset as well as a significantly prolonged clinical duration of action.
Pharmaceutical Effects: Neuromuscular junction includes motor nerve terminals and motor endplates. Under physiological conditions, when the transmission of nerve impulses to the motor nerve terminals, causing the fusion of vesicle located at motor nerve terminal with the nerve membrane and further discharge of acetylcholine in the vesicular. After leaving the nerve terminal, acetylcholine binds to the acetylcholine receptors located at motor endplate, causing the open of ion channels, and the influx of Na+, resulting in the depolarization of muscle cell, further triggering muscle contraction. According to the difference of muscle relaxants’ nerve impulse disturbances on neuromuscular binding regions, the muscle relaxants are classified into depolarizing muscle relaxants and non-depolarizing muscle relaxants.
Rocuronium bromide is a kind of non-depolarizing neuromuscular blocking agents with a similar chemical structure as vecuronium and pancuronium. Being similar as other non-depolarizing drugs, it competitively binds to the cholinergic receptor located in the motor nerve terminals for antagonism of acetylcholine. This medicine is fast-acting, but acts more slowly than succinylcholine with a big range of safety. It has a long duration of action and is in dose-dependent manner. Among the non-depolarizing neuromuscular blocking agents, Rocuronium bromide has a most rapid onset with providing an excellent condition for the cannula after intravenous injection for as short as 60 s whose onset time is a bit longer than succinylcholine though, but is two times as fast as vecuronium and tracrium. Therefore, for the inner rapid intubation, Rocuronium bromide is a good alternative to succinylcholine. However, succinylcholine has a short duration (typically less than 10min) which is much shorter than this product which can last for at least 30min. In this perspective, vecuronium tracrium is similar as atracurium. Compared with other muscle relaxants, the inhibition effect of Rocuronium bromide on motor nerve terminal is weaker than that of d-tubocurarine chloride and pancuronium, but similar as vecuronium. Intravenous anesthesia does not affect the neuromuscular blocking effect of the product nor influence the process.
The median effective dose for children (ED50) and 95% effective doses are 170, 303μg/kg, respectively. After injection of the product for 600μg/kg, the onset time of 90% and 100% neuromuscular blocking are 0.8 and 1.3min, respectively. 25% recovery of neuromuscular conduction requires a time of 27min. Elderly patients (over 70 years) has a similar onset time with young people, but has a prolonged reaction time, a reduced plasma clearance rate and volume of distribution. Kidney transplant patients with renal failure have a longer volume of distribution and elimination half-life for this product than normal person. But there have been no evidences of prolonged intramuscular nerve blocking effect. For the neuromuscular blockage onset time of intravenous injection of this product for 0.6mg/kg, it is longer for patients suffering liver cirrhosis than normal patients (158s ± 56s to 108s ± 36s) with the elimination half-life being 97min ± 37min and 88min ± 18min, respectively.
Uses: 1. It is a kind of muscle relaxants and a kind of non-depolarizing neuromuscular blocking agents. It is used as the adjuvant drugs for general anesthesia and conventional intubation of both inpatient and outpatient. It can keep the muscle relaxation during the process of mechanical ventilation and surgery. 2. It is used as a kind of skeletal muscle relaxants (non-depolarizing)
Chemical Property: Off-white Solid
Uses: A non-depolarizing neuromuscular blocker used in anesthesia to help insert breathing tubes.
Uses: Aminosteroid, competitive neuromuscular blocker
Description: Rocuronium bromide is a short-acting nondepolarizing steroidal neuromuscular blocker introduced in the U.S.A as Zemuron and in the United Kingdom as Esmeron. k is indicated for use as an adjunct to general anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation. Rocuroniurn bromide has a significantly more rapid onset than other intermediate acting neuromuscular blockers, comparable to succinylcholine but with a very stable cardiovascular profile and has an improved side effect profile. It has been reported that good to excellent intubation conditions were achieved only one minute after a bolus dose of 600μg/kg of rocuronium bromide. It has a short duration of action, therefore, is useful for rapid sequence intubation without unacceptable delays in the spontaneous recovery of neuromuscular function.