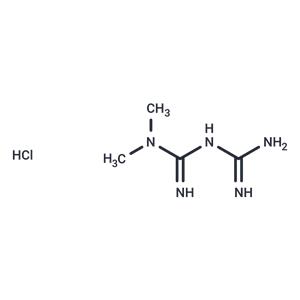
| Name | Metformin hydrochloride |
| Description | Metformin hydrochloride (1,1-Dimethylbiguanide hydrochloride), a widely used anti-diabetic drug, exhibits potential anti-Y properties by inhibiting the proliferation of various Y cells, including colon and prostate. |
| Cell Research | Hepatocytes were isolated from male Sprague Dawley (SD) rats by collagenase digestion. For the AMPK assay, cells were seeded in six-well plates at 1.5 × 10^6 cells/well in DMEM containing 100 U/ml penicillin, 100 μg/ml streptomycin, 10% FBS, 100 nM insulin, 100 nM dexamethasone, and 5 μg/ml transferrin for 4 hours. Cells were then cultured in serum-free DMEM for 16 hours followed by treatment for 1 hour or 7 hours with control medium, 5-aminoimidazole carboxamide riboside (AICAR), or metformin at concentrations indicated. For a 39-hour treatment, cells for both control and metformin (10 or 20 μM) groups were cultured in DMEM plus 5% FBS and 100 nM insulin, and the fresh control and metformin-containing medium were replaced every 12 hours (last medium change was 3 hours before harvest). After treatment, the cells were directly lysed in digitonin-containing and phosphatase inhibitor–containing buffer A, followed by precipitation with ammonium sulfate at 35% saturation. AMPK activity was determined by measurement of phosphorylation of a synthetic peptide substrate, SAMS (HMRSAMSGLHLVKRR). For ACC assay, the 35% ammonium sulfate precipitate from digitonin-lysed hepatocytes (4 μg each) was used for determination of ACC activity via 14CO2 fixation in the presence of 20 mM citrate as done previously. For fatty acid oxidation, the oxidation of 14C-oleate to acid-soluble products was performed as done previously, but in medium M199 in the absence of albumin [1]. |
| Animal Research | Oral gavage was used to administer 1 ml of metformin (100 mg/ml) or water alone to male SD rats (300–350 g, n = 7–8). Rats were treated once or twice a day for 5 days. Rats were starved for 20 hours and then re-fed for 2 hours before the final dose; 4 hours after the final dose, the animals were anesthetized and livers rapidly removed by freeze clamping followed by blood withdrawal. RNA was prepared from the freeze-clamped liver by RNA isolation reagent. Nuclear extracts were prepared from a pool of seven rat livers. Glucose levels were determined using the standard glucose oxidase assay kit; β-hydroxybutyrate concentrations were assayed by measuring the reduction of NAD to NADH with a standard assay kit. FFA levels were measured with the assay kit [1]. MCF10A-ER-Src cells (5 × 10^6) were injected into the right flank of 18 female nu/nu mice, all of which developed tumors in 10 d with a size of ~100 mm^3. The mice were randomly distributed into six groups (three mice/group) that were untreated or treated by intratumoral injections every 5 d (four cycles) with 1 mg/kg or 4 mg/kg doxorubicin, 200 μg/mL metformin (diluted in the drinking water), or the combination. In another experiment, LNCaP and DU145 prostate cancer cells (5 × 10^6) were injected into the right flank of 12 female nu/nu mice, all of which developed tumors in 10 d with a size of ~75 mm^3. The mice were randomly distributed into four groups that were untreated or treated by intratumoral injections every 5 d (four cycles) with 4 mg/kg doxorubicin and/or 200 μg/mL metformin. In another experiment, A375 and MDA-MB-435 melanoma cells (7 × 10^6) were injected into the right flank of 12 female nu/nu mice, all of which developed tumors in 10 d with a size of ~50 mm3. The mice were randomly distributed into four groups that were untreated or treated by intratumoral injections every 5 d (four cycles) with 10 mg/kg cisplatin and/or 200 μg/mL metformin.Finally, SNU-449 liver cancer cells (10^7) were injected into the right flank of 12 female nu/nu mice, all of which developed tumors in 10 d with a size of ~50 mm^3. The mice were randomly distributed into four groups that were untreated or treated by intratumoral injections every 5 d (four cycles) with 10 mg/kg cisplatin and/or 200 μg/mL metformin. Tumor volume (mean ± SD) was measured at various times after the initial injection [3]. |
| In vitro | METHODS: Ovarian cancer cells A2780 and SKOV3 were treated with Metformin hydrochloride (0.001-50 mM) for 24-48 h. Cell viability was assayed using the MTS
RESULTS: Micromolar concentrations of Metformin did not statistically reduce the viability of the A2780 or SKOV3 cell lines. At 48 h, millimolar concentrations resulted in cell death. [1]
METHODS: Human colorectal cancer cells HCT29 were treated with Metformin hydrochloride (0.6 mM) for 90 h. Cell motility was detected using the wound healing assay and chamber invasion assay.
RESULTS: Metformin inhibited the migration and invasion of HCT29 cells, and Metformin decreased the motility of tumor cells. [2] |
| In vivo | METHODS: To model Metformin-induced diarrhea, Metformin hydrochloride (125-500 mg/kg) was administered orally to healthy and diabetic obese db/db C57BL/6J mice twice daily for thirteen days.
RESULTS: Metformin at 1000 mg/kg/day significantly increased fecal water content. Although no diarrhea symptoms were observed in healthy C57BL/6J mice, the same dose of Metformin induced severe diarrhea in diabetic obese db/db mice. [3]
METHODS: To investigate the protective effect of Metformin in radiation injury, Metformin hydrochloride (200 mg/kg once daily for three days) was administered orally to BALB/c mice, which were then exposed to 6-8 Gy of gamma radiation.
RESULTS: When administered prior to exposure to radiation, Metformin prolonged the survival of mice exposed to 8 Gy-TBI and increased the survival of mice exposed to 6 Gy-TBI. Pretreatment with Metformin attenuated radiation damage. [4] |
| Storage | Powder: -20°C for 3 years | In solvent: -80°C for 1 year | Shipping with blue ice/Shipping at ambient temperature. |
| Solubility Information | H2O : 193.21 mM, Sonication is recommended.
DMSO : 50 mg/mL (301.88 mM), Sonication is recommended.
|
| Keywords | type | sensitivity | respiratory | Mitophagy | Mitochondrial Autophagy | mitochondrial | Metformin hydrochloride | Metformin Hydrochloride | Metformin | liver | insulin | Inhibitor | inhibit | diabetes | chain | blood-brain | barrier | Autophagy | AMPK | AMP-activated protein kinase | 1,1-Dimethylbiguanide Hydrochloride | 1,1-Dimethylbiguanide | 1, 1-Dimethylbiguanide Hydrochloride |
| Inhibitors Related | Stavudine | Aceglutamide | Cysteamine hydrochloride | Sodium 4-phenylbutyrate | Hydroxychloroquine | Guanidine hydrochloride | Valproic Acid | Paeonol | Naringin | Alginic acid | Gefitinib | Chitosan oligosaccharide |
| Related Compound Libraries | Bioactive Compound Library | Kinase Inhibitor Library | EMA Approved Drug Library | Anti-Cancer Clinical Compound Library | Drug Repurposing Compound Library | Neuroprotective Compound Library | Inhibitor Library | FDA-Approved Drug Library | Anti-Cancer Approved Drug Library | Anti-Aging Compound Library | Bioactive Compounds Library Max | Anti-Cancer Drug Library |

 United States
United States