| Curative for Major Depression Disorder |
Vortioxetine is a new drug for treating depression, jointly developed and researched by the Danish Lundbeck (Lundbeck) and Japanese Takeda. In September 30, 2013, It is approved by the U.S. Food and Drug Administration (FDA) to enter into market with the brand name of Brintellix, for Major Depression Disorder
(MDD) treatment.
In October 2013, the European Medicines Agency (EMA)’s subordinate agency: Committee for Medicinal Products for Human Use (CHMP) recommended that vortioxetine for the treatment of severe depression should be licensed in the European market and be launched into the European market in January 2014.
MDD features mood changes and a series of other symptoms, which have a great impact on the patient's ability to work, sleep, study, eat and enjoy the current happiness. Depressive symptoms can recur many times in life, but some patients may experience only once.
Vortioxetine, mainly by increasing the concentration of serotonin (5-HT) in the central nervous system (CNS), exerts antidepressant effects. Compared with other selective serotonin reuptake inhibitors (SSRIS) or serotonin-norepinephrine reuptake inhibitors (SNRIS), vortioxetine almost has no effect on norepinephrine and dopamine neurons. A number of clinical trials have demonstrated the efficacy, safety and tolerability of vortioxetine in the treatment of MDD.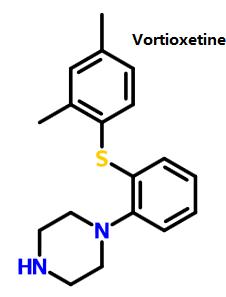 Figure 1 shows the structure of vortioxetine. Figure 1 shows the structure of vortioxetine. |
| Mechanism of Action |
Vortioxetine is a small molecule piperazine sulfide. WHO w classifies it as antidepressants (N06A). The drug classification system of European Pharmaceutical Market Research Association (EPhMRA) classifies it as hypnotic / sedative drugs (N5B), antidepressants and mood stabilizers (N6A). Currently, depression is thought to be associated with a decrease in 5-HT activity, and decreased activity of norepinephrine (NE) and dopamine (DA) is thought to be associated with depression.
Vortioxetine is a potent serotonin reuptake inhibitor. In human body it has high affinity with serotonin trans-porter (Ki=1.6 nmol - L - 1). But it almost has no affinity with norepinephrine transporter (Ki=113nmol - L-1) and dopamine transporter (Ki= 1000nmol - L - 1). At the same time, it is also a 5-HT1A receptor agonist and 5-HT1B receptor partial agonist, 5-HT1D, 5-HT3 and 5-HT7 receptor antagonist and 5-HT uptake inhibitor. Animal studies have shown that in rats, vinpocetine through interaction on these receptors, will increase depression related brain regions -- the level of the ventral hippocampus, prefrontal cortex extracellular serotonin , dopamine, norepinephrine, acetylcholine and histamine, at the same time it is also regulating the function of y -GABA (γ-aminobutyric acid) and glutamatergic neuron, thus exerting the effect of antidepressant. |
| Pharmacokinetics |
The relative molecular weight of vortioxetine is small, and the plasma protein binding rate is 98 percent, which is not related to plasma concentration. It is widely distributed outside the cell and the apparent distribution volume is about 2600 L. Daily oral administration is 2.5 ~ 60mg, showing the linear pharmacokinetic characteristics in proportion to dosage of administration. Bioavailability is 75 percent and generally after 2 weeks of taking vortioxetine, its concentration will be stable in blood. Cmax is 7 to 11 hours. Vortioxetine is metabolized mainly by oxidation and glucuronidation . After a single oral administration of the radioisotope labeled vortioxetine, about 59 percent of it is excreted through the urine, and about 26 percent were excreted through the feces. There was almost no original vortioxetine 48 hours after administration of the drug. The complete metabolism in body requires about 66 hours. The oxidation is mainly completed through cytochrome P450 enzyme (CYP). The involved CYP includes CYP3A4/5, CYP2C19, CYP2C9, CYP2A6, CYP2C8, CYP2B6 and CYP2D6. Among them, CYP2D6 is the key enzyme which catalyzes and produces the main metabolite of duloxetine carboxylic acid. The drug concentration of CYP2D6 in the plasma with slow metabolism is twice higher than that of CYP2D6 in the plasma with the fast metabolism. |
| Drug Interaction |
- In the different experiment and researches using healthy volunteers as subjects, vortioxetine will be co-administered respectively with CYP2D6 inhibitor bupropion, CYP2C9/CYP2C19/CYP3A inhibitor fluconazole or CYP3A/ permeability glycoprotein (P-gp) inhibitor ketoconazole. The vortioxetine’s bioavailability will increase. Therefore when vortioxetine and strong CYP2D6 inhibitors (such as bupropion, fluoxetine, paroxetine and quinidine) are co-administered, the dosage should be halved.
- When vortioxetine and strong CYP inducers (rifampicin) are co-administered, its bioavailability will be reduced. Therefore when vortioxetine is co-administered with rifampicin or other strong CYP inducers (such as carbamazepine, Phenytoin sodium), the dosage should be increased, but the maximum dosage should not be three times higher than the normal dose.
- In addition, the use of 5-HT drugs itself is a risk factors of incurring abnormal bleeding. Therefore when vortioxetine is co-administered with aspirin, nonsteroidal anti-inflammatory drugs or other drugs affecting blood coagulation, special attention should be drawn to the abnormal bleeding of patients.
- Considering the functional mechanism of vortioxetine and potential toxicity of serotonin, so when it is co-administered with other drugs affecting 5-HT neurotransmitter systems (such as SSRIs, SNRIs, and triptans, buspirone, tramadol and tryptophan products), lt is likely to occur 5-HT syndrome. Therefore, close attention should be paid to the risk of 5-HT syndrome when it is used in combination with such drug. Once the 5-HT syndrome occurs, all such drugs should be discontinued immediately.
- Similar to the above reasons, monoamine oxidase inhibitors (MAOIs) are prohibited from being used in combination with MAOIs. MAOIs can not be administered within 21d after discontinuation of vortioxetine, and vortioxetine can not be administered within 14d after discontinuation of MAOIs. Because the combination of both will increase the risk of 5-HT syndrome in patients.
|
| Synthesis |
- 2,4-dimethyl-1- iodo-benzene reacts with 2- bromophenyl thiophenol and Bis(dibenzylidene acetone)palladium, under sodium tert-butoxide’s catalysis to generate vortioxetine
- 2,4- dimethyl thiophenol and 2- bromo benzene and piperazine(1-BOC-piperazine) react under the catalysis of Bis(dibenzylidene acetone)palladium , 1, 1'- linked naphthalene -2, 2'- bis diphenyl phosphine and sodium tert-butoxide to generate vortioxetine.
 |

 China
China




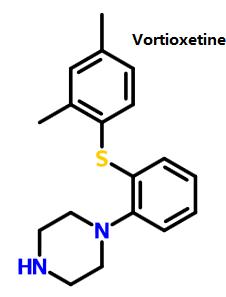 Figure 1 shows the structure of vortioxetine.
Figure 1 shows the structure of vortioxetine.

