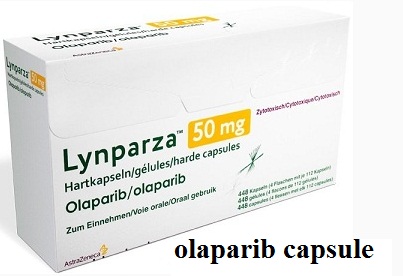
Olaparib
- Product NameOlaparib
- CAS763113-22-0
- CBNumberCB02473811
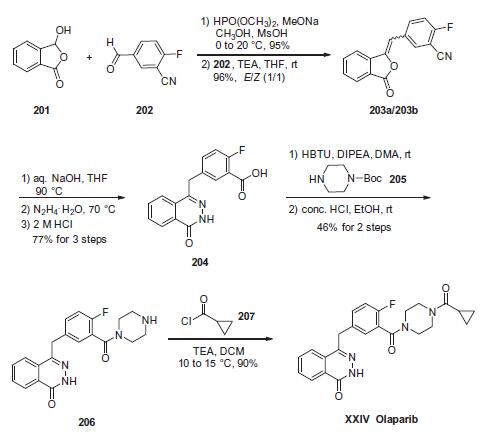
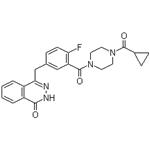
- MFC24H23FN4O3
- MW434.46
- EINECS642-941-5
- MDL NumberMFCD13185161
- MOL File763113-22-0.mol
- MSDS FileSDS
Chemical Properties
| Density | 1.43 |
| storage temp. | -20°C |
| solubility | Soluble in DMSO (up to 33 mg/ml) or in Ethanol (up to 1.7 mg/ml) |
| pka | 12.07±0.40(Predicted) |
| form | solid |
| color | Off-white |
| Stability | Stable for 2 years from date of purchase as supplied. Solutions in DMSO or ethanol may be stored at -20°C for up to 1 month. |
| InChIKey | FDLYAMZZIXQODN-UHFFFAOYSA-N |
| SMILES | C1(=O)C2=C(C=CC=C2)C(CC2=CC=C(F)C(C(N3CCN(C(C4CC4)=O)CC3)=O)=C2)=NN1 |
| CAS DataBase Reference | 763113-22-0 |
| NCI Dictionary of Cancer Terms | AZD2281; olaparib |
| FDA UNII | WOH1JD9AR8 |
| NCI Drug Dictionary | olaparib |
| ATC code | L01XK01 |
| UNSPSC Code | 12352200 |
| NACRES | NA.77 |
Safety
| Symbol(GHS) |

|
|||||||||
| Signal word | Danger | |||||||||
| Hazard statements | H314 | |||||||||
| Precautionary statements | P501-P260-P264-P280-P303+P361+P353-P301+P330+P331-P363-P304+P340+P310-P305+P351+P338+P310-P405 | |||||||||
| Risk Statements | 22-38-37-36 | |||||||||
| Safety Statements | 24/25-37/39 | |||||||||
| HazardClass | IRRITANT | |||||||||
| HS Code | 29339900 | |||||||||
| NFPA 704: |
|